7 Supraventricular Arrhythmias
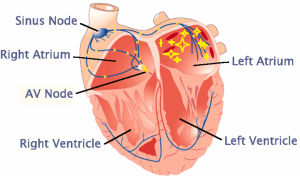
Supraventricular, or “above the ventricle” is an area including the AV node and the atria. Typically, the SA node dominates the pacing of the timing of both atrial and ventricular pacing (by way of AV node signal transfer from atria to ventricle). However, alterations in electrolytes, changes in sympathetic or parasympathetic activity, accessory pathways between the atria and ventricles other than the AV node and areas of damaged tissue in the atrial can create opportunities for other potential pacemakers to become dominant. This chapter will examine common supraventricular arrhythmias that exercise science professionals may encounter in their work with cardiac patients.
AV node- Junctional rhythm
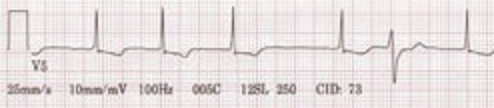
AV node tissue by itself has a typical pacemaker rate of about 50 beats per minute. So typically, the faster pacing SA node controls rate. Slower rate (less than 60) “junctional rhythm” pacing or with a stimulated AV node faster rate “accelerated junction rhythm” (rate 60-100) and even “junctional tachycardia” (rate over 100) are possible.
Because the atria and the ventricle are being stimulated at the same time (like a pebble dropped in a pond; waves move outward in all directions), the atrial depolarization wave can have a range of looks. Often, we see “retrograde P waves” or upside-down p waves, often quite close to the QRS complex. However, in other cases the wave does not propagate into the atrial and we do not see any p wave:


Test yourself. What would you call this rhythm?

Rate? _______________ P waves (Upright? Retrograde? Not present?)
Interpretation? (junctional rhythm, accelerated junctional rhythm, junctional tachycardia)
Summary– so the key to identifying a junctional rhythm is the narrow QRS complex, the rate, and whether there are retrograde or missing p waves.
AV node- accessory circuit- another way into the ventricle! Re-entrant arrhythmia: Supraventricular Tachycardia
In normal heart tissue there is only one pathway from the atria into the ventricle, and that is the AV node. However, there can be accessory pathways that exist in the same area as the AV node and bundle of His (i.e. bundle of Kent). These accessory pathways create a situation where a premature beat in the right location can create a sudden, rapid increase in heart rate.
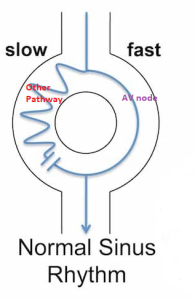
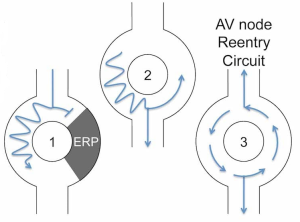
Steps in the creation of a reentrant circuit.
Step 1. A well-timed premature beat (PAC) in close proximation to the pathways occurs. The AV node is still in refractory, so it has yet to reset so it can receive the signal. However, the accessory path has a very brief refractory period and has already reset, so the signal passes down the other path.
Step 2. The signal comes out of the pathway at the same time as the AV node is reset, so the signal is both conducted to the ventricle but also conducted backwards through the AV node.
Step 3. A circuit is created between the accessory pathway and the AV node, causing a very rapid signal that presents any signal from the SA node getting through. The rate of the circuit can be very high (over 200bpm) and patients can become symptomatic (dizziness, palpitations, anxiety).
Supraventricular Tachycardia (SVT)
SVT is a reentrant tachycardia, with a rate typically between 140-250bpm. It may be associated with some type of stimulation, such as caffeine use, alcohol, stimulant drugs and even exercise. Often it has a rapid onset. Patients with this condition typically will have to manage it throughout their life. SVT may resolve itself, but often other treatments may be used:
- Vagal maneuvers (cough, bear down, carotid massage) to kick patient back to sinus rhythm.
- Treatment with the drug Adenosine (blocks AV conduction, increases refractory).
- Calcium channel blocker drug (av node conduction block).
- In some cases, catheter ablation procedures are used to isolate the accessory pathway.
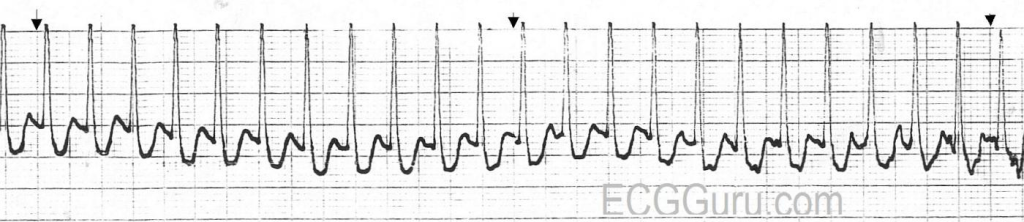

In summary, AV node-related supraventricular tachycardias have high rates, often no p waves present, but can be medically treated along with lifestyle changes to avoid triggers. The exercise science professional should study the case history of the patient to understand triggers and symptoms that are present with the condition.
Supraventricular Tachycardias Within the Atria: Atrial fibrillation and Atrial Flutter
Atrial fibrillation is a common heart arrhythmia, with the Centers for Disease Control and Prevention estimating that by 2030 more than 12.1 million Americans will have this condition. It is more prevalent in individuals of European decent, and is more common in women, however this may be because age is a key factor in developing Afib (and women live longer than men).
Key risk factors include: Age, High blood pressure, Obesity, Diabetes, Heart failure
Note that many of these risk factors result in alterations in the atria. Nerves around the pulmonary vein can serve as a source of sporadic firing of cells, and the result can be a spread of random firing across all the atria, resulting in no actual atria contraction, but rather a quivering (fibrillation).
Blood flow through the heart in Afib
With a lack of atrial contraction, flow from the atria into the ventricles is passive (no atrial kick), resulting in a reduced cardiac output, especially during exercise (less time for passive filling of ventricle). Additionally, blood can pool in areas of the atrial, such as the left atrial appendage, resulting in the formation of blood clots. This is one of the biggest risks of atrial fibrillation.
Watch this video simulation of atrial fibrillation. Be sure to select atrial fibrillation from the menu in the lower right corner of the video.
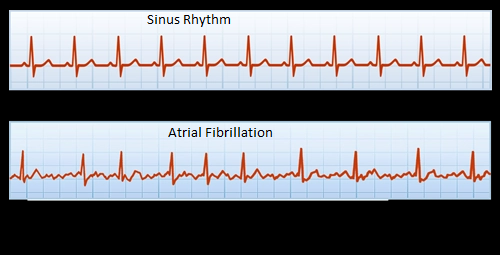
Atrial fibrillation on the ECG
With random firings from many cells in the atrial, there is no distinct P wave in Afib. Instead, you will see chaotic firing, which may be pronounced or very fine. Additionally, passage through the AV node will be random, so the ventricular response will show an irregular rhythm. The rate may be fast or slow, depending on the response rate of the AV node.
Atrial Fibrillation Treatment
Long term atrial fibrillation modifies the shape of the atria, making the condition permanent, so early intervention is essential. See Chapter 4 for a more complete description of afib treatments, which include:
- Cardioversion
- Drugs to reduce AV node condition (reduce rate) and possibly reconvert back to sinus rhythm
- Catheter ablation around pulmonary veins
Additionally, controlling the formation of blood clot formation is essential, so patients are on thrombolytic therapy and may also undergo other procedures to reduce clot formation to prevent stroke or infarction (Chapter 4).
Atrial Flutter
Atrial flutter is another situation where there is a reentrant signal causing a rapid, cyclic firing at a very fast rate. In the case of atrial flutter, it occurs most often in the right atrium and is due to some type of lesion or ischemic tissue in the atria that is serving as the slow conducting, fast refractory reentrant pathway.
As you look at the ECG, note the “Saw Tooth” characteristics of many P waves (referred to as “F” waves or flutter waves. The reentrant firing is so fast that not all the flutter waves get through the AV node, because it is refractory for some of the time. Therefore, you may see variations in the number of non-conducted or blocked flutter waves, followed by a conducted wave and a QRS complex.
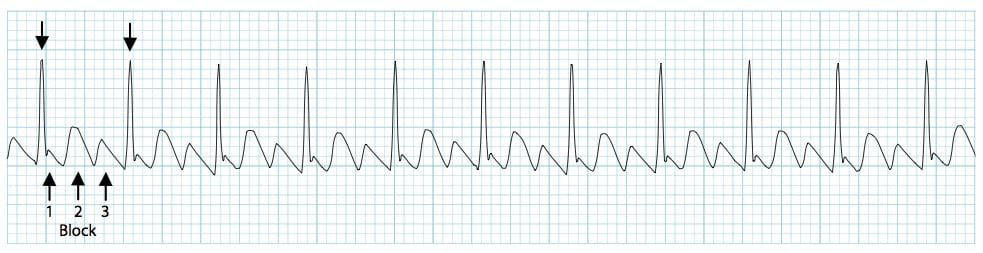

Atrial flutter and atrial fibrillation often have similar treatment plans (medication, cardioversion, ablation) and carry the risk of blood clot formation. The exercise science professional should review the current treatment plan for their atrial fibrillation or atrial flutter patient so that you are aware of factors related to their condition.
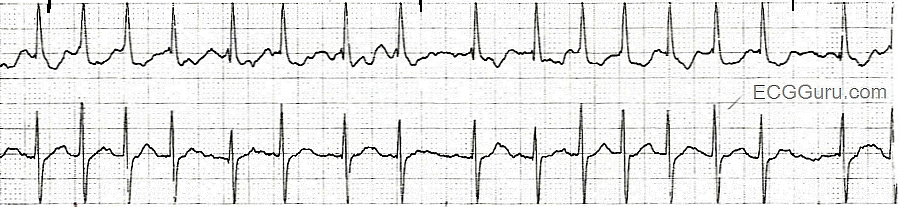
Mini Quiz! Can you identify? (you may have to compute rates)


Answers (you didn’t peek did you?)
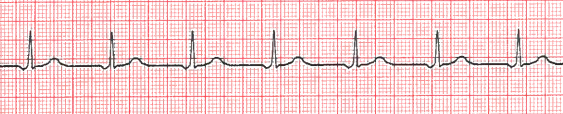
Figure 14: Accelerated Junctional Rhythm
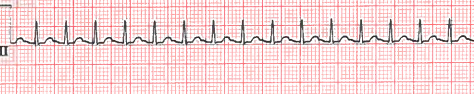
Figure 15: Atrial Flutter
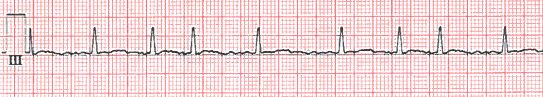
Figure 16: SVT (supraventricular tachycardia)
Figure 17: Atrial Fibrillation
Figure 18: Sinus Tachycardia
Selected Sources
Goldberger’s Clinical Electrocardiography: A simplified approach 10th ed. Goldberger A., Goldberger, Z, Shvilkin A. Elsevier pub. ISBN-10 0323824757 2023.
Clinical Exercise Electrocardiography – Levine S., Coyne B., Colvin L. Jones & Bartlett Learning Pub. ISBN-10 1284034208 2015.
Centers for Disease Control and Prevention. Atrial Fibrillation: https://www.cdc.gov/heartdisease/atrial_fibrillation.htm#:~:text=More%20than%20454%2C000%20hospitalizations%20with%20AFib%20as%20the,been%20rising%20for%20more%20than%20two%20decades.%207
Video links used in Chapter 7
Animation of atrial fibrillation ( Be sure to select atrial fibrillation from the menu in the lower right corner of the video): https://watchlearnlive.heart.org/index.php?moduleSelect=arrhyt
Procedure to destroy tissue that is abnormal or malfunctioning. In cardiac procedures it is often a catheter procedure, using heat, cold or electrical energy. Common to atrial fibrillation treatment.
A timed defibrillation procedure where the depolarization shock is synchronized with the ventricular systole to prevent inducing dangerous arrhythmias. It is used in cases of atrial fibrillation, flutter and SVT. Chemical cardioversion is also possible with medications such as flecainide, amiodarone or propafenone.
