13 Outpatient Cardiac Rehab: Phase II
Program Goals and Exercise Prescription Guidelines
There is clear evidence that outpatient cardiac rehab reduces mortality and morbidity in patients that participate. In fact, there is a linear reduction in mortality in congruence with the increased participation . Data show that mortality can be reduced by as much as 30% for those who participate. Unfortunately, only about 20% of those that need outpatient cardiac rehab participate in rehab. Issues such as transportation, delays in referral, patient adherence, lack of buy-in as well as a reduced infrastructure to accommodate all the patients play a role in the reduced participation.

Hospitals continue to expand their outpatient programs to accommodate the ever-growing volume of patients.
The ideal approach to preventing patients who have cardiovascular disease from having a reoccurrence of an event or progression of the disease is known as secondary prevention. Secondary prevention involves an individualized program addressing a wide range of prevention programming:
- Physical training to improve functional capacity (MET capacity) and improved strength and flexibility.
- Focused pharmacology to help address the risk factors contributing to the disease.
- Nutritional education to improve the diet and impact risk profiles.
- Stress management, smoking cessation, and other lifestyle modifications to improve outcomes.
These are no easy tasks! Realize the typical patient has a significant risk profile, is probably inactive, overweight and has lived the lifestyle that got them to their event for many years. Exercise science professionals in cardiac rehab are a very important part of their lifestyle change! You will be the essential link to establish consistent and important communication with the patient, and you will serve as a coach and guide to help them make lifestyle changes to change their path towards a healthier way of life.
Initial Patient Assessment
Initial patient assessments will of course include a review of the medical records, which includes surgical history, any events, and comorbidities and if available any post-surgical care. Assessments may include 12 lead ECG, stress test data, angiography, description of surgeries and any other device (i.e pacemaker) or treatment (i.e catheter ablation?).
Risk factors– don’t ignore risk factors! Yes, they have had an event, but now more than ever risk factors need focused attention when planning the secondary prevention program.
Medications– What medications were they on initially? What about current? This will provide patient information and help you when planning education for the patient.
Functional ability– Can they walk? Will they need to cycle instead? Any orthopedic issues? Injuries, surgical wounds that are still healing? Assessing functional ability can inform the modes of exercise you choose.
Day 1 exercise– Unfortunately, the day the patient arrives you may or may not have all of the information you need. You may have exercise data, or not. So, the first day exercise may be a lower intensity assessment to see how the patient responds to exercise. It may be limited to no higher than resting HR + 20 or + 30, and then gather RPE, heart rate, blood pressure and rate pressure product information.
Individualized Training Program (ITP)
Aerobic Training- The initial training program will identify parameters for Frequency of exercise, intensity, duration as well as mode of training.
Example:
Patient will begin with treadmill walking at 2.7 METS, Heart rate range 115-125bpm, RPE 11-13
Duration– 15 minutes (initial)
Frequency: Phase II 3 days per week. Home exercise 2 days per week
Cycling at 2.3 METs, RPE 11-13 HR 115-125
Duration– 15 minutes (initial)
These are hypothetical intensities and durations of exercise. Each patient will be different. Be attentive to their response to exercise, and follow-up with them on subsequent session to learn how they felt afterward. Some may feel fine, while others are quite fatigued. There is a bit of an art to this science, so use your emotional intelligence as well as science!
Home exercise might have a different plan since the patient is unmonitored. Perhaps lower intensity and focus more on RPE guiding intensity.
Flexibility Training
Flexibility exercises should be designed to help the patient improve daily activity by increasing joint range of motion. Upper body, lower back and legs stretching exercises, held to the point of tightness. Avoid breath holding or valsalva, as this elevates blood pressure. Hold for 10-30 seconds and repeat 4 times for each stretch.
| Name of Method | Formula | Population that may be suited for method |
| Percent Heart Rate Method
Heart rate above resting limited |
Max HR x desired training percent (in decimal form)
i.e max HR of 200x .70= 140bpm 70% of max HR
+20bpm above resting HR (MI patients, + 30 (CABG) |
Apparently healthy population. often HR Method used on exercise devices for HR training zones
Patients coming from Phase I or patients where there is no exercise test information available |
| RPE method
|
On a 6-20 scale:
Less than 12 light (less than 40% HRR) 12-13 somewhat hard (40-59% HRR) 14-16 hard (60-80% HRR) |
Peak HR is not known, and HR is an unreliable (afib, patients taking beta blockers, or recently placed on beta blocker) |
| Heart rate reserve method (Karvonen)
|
[(Max HR-resting HR) x intensity (decimal)) +rest HR Range is somewhere between 40-80% HRR
Note: don’t forget to add back the resting HR at the end to get the correct answer! |
Peak HR is known, patient has had an exercise test performed and responses through the range of intensity is known. |
| VO2 reserve method |
[(Peak VO2-resting VO2) x intensity (decimal)) +rest VO2
|
Peak VO2 is known, patient has had an exercise test performed and responses through the range of intensity is known. |
| Ischemic Threshold Method | Identify the heart rate and rate pressure product that coincides with the ST depression and/or angina symptoms. HR intensity should be at least 10 bpm below the ischemic threshold | Patients with stable angina, predictable at a rate pressure product (HRx SBP) |
HR= Heart Rate; HRR= Heart rate reserve
Resistance Training
For some patients, resistance training is NOT indicated. For example, post-surgical patients who have lifting restrictions should not begin resistance exercises until cleared from these restrictions. CABG patients need to heal the sternal incision and bone, so lifting is not indicated for them until the sternum has healed (8-10 weeks). Other patients may have conditions that prevent incorporation of resistance training (stroke related, other cardiac issues made worse by added pressure)
Be aware of the effect lifting on rate pressure product. Breath holding or valsalva can exacerbate these increases in RPP, leading to the patient exceeding their ischemic threshold. Therefore, when resistance training is introduced, be sure to teach the proper methods of lifting, both skill in lifting as well as breathing out during the exertion. They need to learn to not breath hold.
When resistance training is introduced the recommendations according to the American College of Sports Medicine are:
Frequency– 2-3 non-consecutive days per week
Intensity– 10-15 repetitions of each exercise without significant fatigue. RPE 11-13, 40-60% of 1 rep max
Time– 1-3 sets, 8-10 different exercises focused on major muscle groups.
Be sure to start light, teach them properly so that they can safely execute the exercise. Unlike healthy individuals, DO NOT have them lift to fatigue. It is important to build some strength, but endurance as well.
A typical exercise session
The patient arrives at the outpatient cardiac rehab center. Upon arrival, they obtain body weight, prepare their skin and apply electrodes to connect to the telemetry ECG system, get their exercise shoes on and have a seat for a few minutes so that you can get resting measures.
- Resting measures may include:
- Resting heart rate and ECG rhythm
- Resting Blood pressure
- Resting Blood Glucose (if diabetic)
- Check to determine if they have taken normal medications for the day
- Check on any activities, symptoms since the last visit. Just have a chat with them!
 |
 |
The exercise space looks much like a gym you would see anywhere else, but perhaps smaller. It might have a small track, a number of treadmills, Nustep training devices, cycle ergometers and perhaps some light weights and bands for resistance training. Classes may range in size from 5-10 depending on staffing and the size of the facility.

The exercise session is often multimodal, with patients moving from treadmill to cycle and perhaps to NuStep (if cleared for upper body exercise) exercising both upper and lower body. Blood pressure, ECG and RPE are monitored and recorded, along with the MET intensity on each mode.
Cool-down sessions may consist of light exercise, stretching and continued monitoring of ECG, blood pressure and any symptoms that may present.
Functional Capacity test to check progress
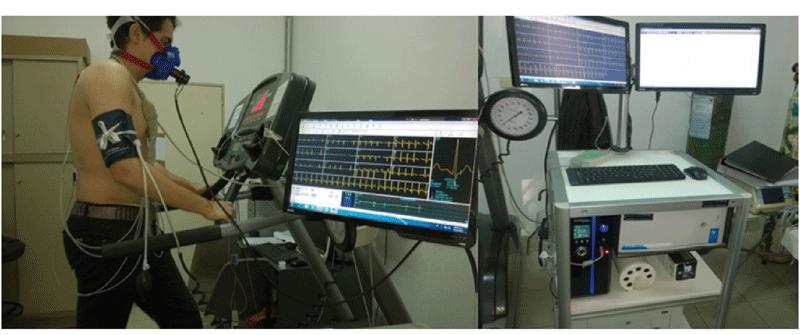
Depending on the facilities of the hospital, patients may complete a functional capacity test, typically on a treadmill or a cycle ergometer. Often the Bruce protocol is used, but other protocols, such as modified Bruce or Naughton protocols may also be used. The patient is connected to a 12 lead ECG and often a metabolic cart is also used to get a true measure of oxygen consumption. Once the results of the test are known, and updated ITP (individualized treatment plan) can be made, and the patient begins to feel more confident in their progress and fitness.
Exercise Considerations for Different Conditions
Each patient will have individualized programs created, and there will be some common focus points for some conditions. Here are some brief descriptions of exercise programming considerations for different types of phase II patient conditions.
CABG and sternotomy
Following surgery, the closed sternum is strong enough that free arm movement is possible and should be encourage with rage of motion exercises that keep the arms close to the body to reduce unexpected torque on the sternum from an outstretched arm hitting a resistance.
It is important to teach the patient how to sit and stand from a seated position without using the arms, as loading arms with body weight is very painful and ill-advised. Use of a pillow when coughing to reduce sternal pain should be taught.
Heart Failure
Considerations with the heart failure patient will depend on the resting ejection fraction and MET capacity. Symptoms of dyspnea and fatigue along with signs of edema and low Oxygen saturation will be important measures to monitor and guide the exercise plan. These patients are typically on very strict low sodium diets and diuretics that control edema. Patient management and education is important for them to learn how to control fluid accumulation and desaturation.
For heart failure patients fitted with a left ventricular assist device (LVAD) be aware that the flow rate of the pump is stronger than the systolic pressure wave. As a result, you will not feel pulses, so traditional heart rate and blood pressures cannot be measured in the same manner. ECG recordings can track heart rate, and flow regulated on the LVAD. ACSM guidelines suggest that mean arterial pressure (MAP) be measured using a doppler probe instead of stethoscope, with resting MAP goal of 70 to 80 mmHg. MAP should rise with increasing work (up to perhaps 90mmHg). RPE of 11-13 is suggested. Be aware of fatigue onset both during exercise and later in the day. It may be advisable to perform intermittent exercise to allow more recovery time during exercise sessions.
Cardiac Transplantation
With only about 3,000 heart transplants performed in the US annually, these patients are not seen too often. The biggest factor for the cardiac rehab professional to consider related to exercise is the fact that the transplant patients’ heart is denervated. That is, there is no parasympathetic and sympathetic nerve innervation, so the pacing rate and rate responsiveness of the patient is compromised. Peak cardiac output is reduced by 20-30 percent, and resting heart rate is elevated (around 100 bpm) without parasympathetic control. Also, during exercise, the only means of accelerating heart rate is via epinephrine release from the adrenal gland. This means that both increases and decreases in heart rate are very slow. Exercise testing protocols should have slow transitions and gradual increases. Exercise sessions should be preceded by a lengthier warm up, with gradual transitions to training intensity. There should also be a longer cool down session to bring the patient back to rest.
Pacemaker and ICD
Pacemakers can be utilized in a variety of ways to establish a desired heart rate and connection between the atria and the ventricle. It is important to understand the type of pacemaker the patient has, so that you understand how it will respond to exercise. Some pacemakers are rate responsive (to exercise) while others are not. Exercise testing of patients with rate responsive pacemakers can provide better information about how the pacemaker adapts to exercise, and exercise programming can be more precise. Some pacemakers have programmed limits, and implantable cardiac defibrillators (ICDs) have upper limits that can trigger defibrillation. Exercise training should stay at least 15 bpm below ICD thresholds for defibrillation. It is essential that you know these limits!
Peripheral Artery Disease
Patients with peripheral artery disease experience intermittent claudication, the pain associated with ischemia in the lower limbs due to a restriction of blood flow. Patients will also have a reduced ankle-brachial index (under .90). It is important to identify functional capacity by identifying symptom onset and pain tolerance of the patient. Intermittent exercise is the only way one can train a PAD patient. They will exercise to the point of pain tolerance, followed by rest to relieve the symptoms. Then they repeat the exercise. Monitoring vitals during exercise and recovery is important. Progress can be noted by the duration of the exercise sessions as well as distance walked.
Pulmonary Disease
There are a wide range of conditions that may be present in pulmonary patients, ranging from asthma, to emphysema, to pulmonary fibrosis. It will be important to understand the nature of the patient’s pulmonary condition and the limitations that it presents. Exercise provides excellent conditioning of the respiratory muscles and may help reduce some symptoms. Patients with COPD may need assistance in training with proper breathing to adequately ventilate (i.e. pursed lipped breathing), and how to maintain good ventilation during exercise. Fatigue, poor breathing and rapid desaturation is a possibility, so you need to monitor the patient’s symptoms (fatigue, dyspnea, anxiety) and signs (oxygen saturation). Patients that experience exercise induced asthma may need a pre-exercise administration of an inhaled bronchodilator (something they should consult with their physician).
Nutrition and Other Programming
The educational component of Phase II may be sessions on non-exercise days or perhaps following an exercise session. Registered dieticians often work with programs to provide nutritional content. This may be in the form of recipes, cooking demonstrations and discussions about nutritional factors such as sodium and how it affects their outcomes. Most nutritional plans are some variations of a Mediterranean diet. Here are two examples:
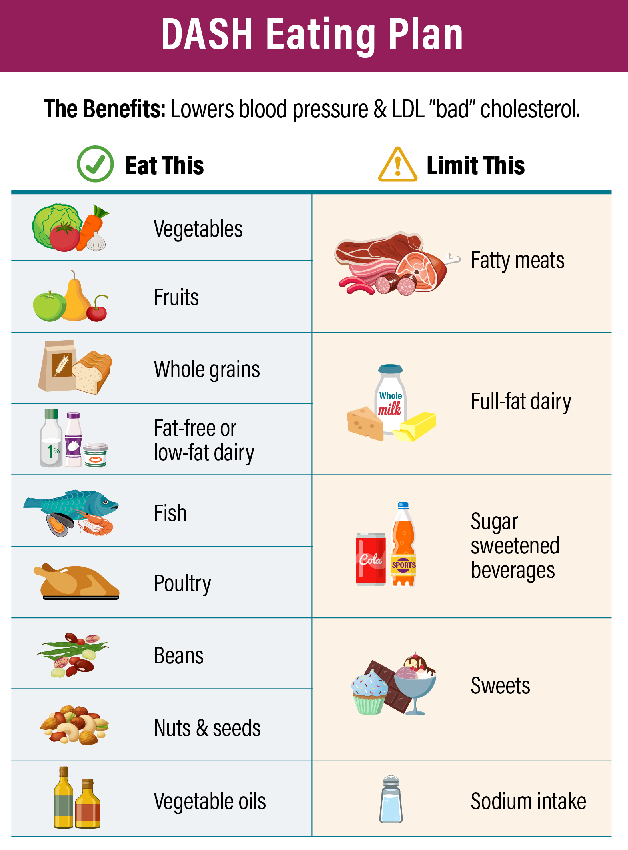
DASH Diet- This acronym means “Dietary Approaches to Stop Hypertension. This is an eating plan that emphasizes lean meats, fish, fruits and vegetables, low fat dairy, and low sodium.
According to the National Heart Lung and Blood Institute a diet plan based on a 2,000 calories day diet would look like this:
| Food Group | Daily Servings |
| Grains | 6–8 |
| Meats, poultry, and fish | 6 or less |
| Vegetables | 4–5 |
| Fruit | 4–5 |
| Low-fat or fat-free dairy products | 2–3 |
| Fats and oils | 2–3 |
| Sodium | 2,300 mg* |
| Weekly Servings | |
| Nuts, seeds, dry beans, and peas | 4–5 |
| Sweets | 5 or less |
*1,500 milligrams (mg) sodium lowers blood pressure even further than 2,300 mg sodium daily.
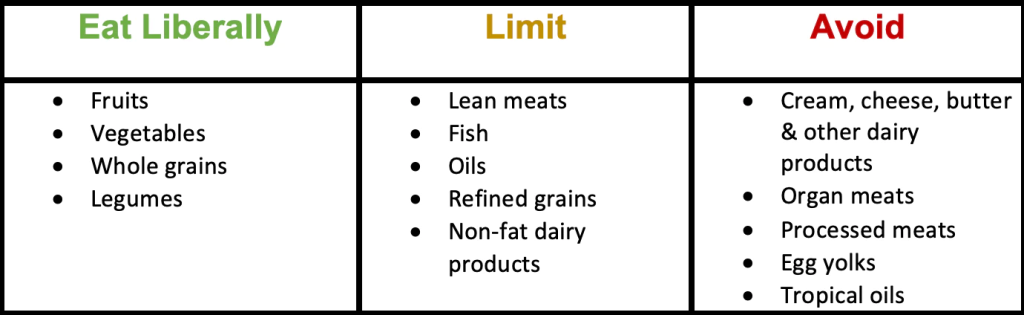
Pritikin Plan: This diet plan is utilized an many cardiac rehab programs and focuses on Fruits and vegetables, whole grains, starchy vegetables, plant-based proteins along with fish and other low saturated fat proteins, and calcium-rich dairy alternatives.
Stress Management
Stress, anxiety and depression are all aspects of daily living, and are often exacerbated by a cardiovascular disease event and subsequent surgery. Management of mental health is an important aspect to address for the phase II patients as they seek to change their lifestyle to one that reduces their risk of a secondary cardiovascular event.
- Activities that may be part of a stress management program in cardiac rehab may include:
- Visualization exercises
- Meditation
- Progressive muscle relaxation
- Stretching
- Self-massage
Along with these techniques patients can learn mindfulness training to better cope with their symptoms and circumstances, helping them deal with the many aspects of their condition that can be a source or stress. These techniques are rarely known by the typical individual, so they can provide useful tools and coping skills moving forward.
Smoking Cessation
A variety of resources and programs are available to help patients quit tobacco use. These can be in support group-type formats, apps, and counseling. Some sources include:
quitSTART- a free smartphone app to help you quit smoking. See www.smokefree.gov
How to Quit Smoking– https://www.cdc.gov/tobacco/campaign/tips/quit-smoking/index.html
Quit Assist Information Resource: https://www.quitassist.com/ (see helpful resources)
Better Breathers Club
This is a group organized by the American Lung Association. Members learn better ways to cope with lung conditions such as COPD, pulmonary fibrosis, and asthma. Meetings are in person or virtual, where trained facilitators provide training to help cope with breathing issues. It is also a support group of individuals to help others manage their disease. *see https://www.lung.org/help-support/better-breathers-club )
Your Turn! Work with your instructor and student colleagues
to complete the Phase II case study below:
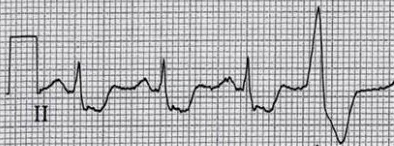
John is a sedentary 47 year old smoker who weighs 245 lbs (111.4kg) and is 5’10” (178cm) tall (BMI?). He was recently admitted to the hospital complaining of chest pain. His cardiac enzymes (Identify________) and protein (Identify _________) were elevated along with ST segment elevation, confirming an acute MI. John was rushed to the cath lab, where it was determined that his LAD was occluded (95%) at the proximal end. He underwent PTCA and stent placement, which was successful. His ejection fraction was 55%. Two weeks have passed and John has arrived to begin phase II cardiac rehab. He recently completed a stress test, terminated at 10:00min due to ECG changes and dyspnea.
Rest HR: 60bpm Rest BP: 142/90 TC- 250mg/dl LDL- 160mg/dl HDL- 35mg/dl
Medications: Tenormin (atenolol), Cardizem (diltiazem), Aspirin
| Stage | Speed | Grade | HR | BP | RPP | RPE | METS | notes |
| I | 2.0 | 0 | 85 | 154/92 | _________ | 11 | _____ | |
| II | 2.0 | 3.5 | 94 | 164/92 | _________ | 13 | _____ | |
| III | 2.0 | 7.0 | 100 | 172/94 | _________ | 15 | _____ | 1 Dyspnea, 1 on angina ST depression 1.5 mm |
| IV | 2.0 | 10.5 |
________ Identify see ecg |
182/96 | _________ | 17 | _____ | 2 Dyspnea, 3 on angina
ECG (see attached) ST depression (identify)_____mm |
Test terminated at 10:00min
Program
- Fill in the rate pressure product (RPP) values, Fill in all “Identify” blanks in the table above.
- Fill in the MET values, either calculate by hand or go to www.ExRx.net
- Use the ECG above to complete the last stage data on the table
- Identify any secondary prevention risk factors that will require addressing in the treatment plan:
- Identify medications: Mechanism of action, why would the patient be on the particular medication? Any effect on HR or BP?
HR prescription- Which Method to use? Let’s try a common one
6. Using Age predicted variables- Calculate heart rate intensity at 60% and 80% HRR (be sure to add the resting Hr at the end of the formula!). Is this an appropriate heart rate prescription based on the data from the stress test? Explain
60% HRR method= __________________
80% HRR method = _________________
Would these heart rate prescriptions above be appropriate? Explain.
7. Choose an appropriate prescription method from Table 1 (this chapter ) and identify appropriate training variables for treadmill walking. Identify the RPP that coincides with the ischemic threshold (use data table above)
| Mode | HR for training | RPE for training | RPP limit (ischemic threshold) | MET Intensity | Speed and grade |
| Treadmill | 10 beat range= ____ to____bpm | RPE = _____ |
_______________________ |
METs = ______ | Speed:_______
Grade:______
|
8. Cycle exercise is also used in training. However stationary cycling uses 10% less muscle mass than treadmill work, so we need to reduce our MET prescription by 10%. Identify the new MET prescription ______________ and the Watt intensity for cycle training ______________________
Please note! These are starting points and you need to monitor the patient for any signs and symptoms that might indicate the prescription is not appropriate. Make no assumptions!
Selected Sources
- ACSM Guidelines for Exercise Testing and Prescription. 11th ed. Wolters Kluwer Pub. 2022.
- Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 5th ed. American Association of Cardiovascular and Pulmonary Rehabilitation. Human Kinetics Pub. 2013.
- AACVPR Cardiac Rehabilitation Resource Manual. American Association of Cardiovascular and Pulmonary Rehabilitation. Human Kinetics Pub. 2006.
- Milani, RV and Lavie, CJ. Impact of cardiac rehabilitation on depression and its associated mortality. Am J. Med. 120, 799-806, 2007.
- Dibben G, Faulkner J, Oldridge N, Rees K, Thompson DR, Zwisler A-D, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database of Systematic Reviews 2021, Issue 11. Art. No.: CD001800. DOI: 10.1002/14651858.CD001800.pub4
- Medina-Inojosa, JR, Grace, SL, Supervia, M, Stokin, G, Bonikowske, AR, Thomas, R, Lopez-Jimenez, F. Dose of cardiac rehabilitation to reduce mortality and morbidity: a population-based study. J. Am Heart Assoc. 2021 DOI: 10.1161/JAHA. 120.021356
- Metabolic Calculations- www.exrx.net (see “Fitness Calculators”)
Measures to reduce the risk of additional heart disease complications in patients with latent disease. These measures can include cardiac rehab, nutrition counseling, stress management, medications, and smoking cessation.
A catheter procedure that is used to destroy tissue that is abnormal or malfunctioning. In cardiac procedures it is often a catheter procedure, using heat, cold or electrical energy. Common to atrial fibrillation treatment.
Exhaling against a closed resistance. This can be as simple as breath holding, or with much more force, like during a heavy lift. For heart patients this can be dangerous, as it also causes substantial increases in blood pressure.
An index of myocardial oxygen use (“work of the heart”). RPP is calculated as heart rate x systolic blood pressure.
Difficulty breathing characterized by breathlessness and a feeling of not being able to get enough air in the lungs to relieve the distress. Causes can include COPD, anxiety, deconditioning, and edema caused by heart failure.
An abnormal accumulation of fluid in the interstitial spaces. The accumulation can occur in the leg (peripheral edema) lungs (pulmonary edema) and the arms and abdomen(ascites).
A value that represents the average pressure in the arteries during a single cardiac cycle. It is calculated as: Diastolic pressure + 1/3 pulse pressure. A blood pressure of 120/80 is a MAP of 93. Below 60-70mmHg MAP cerebral perfusion may be inadequate and the patient may lose consciousness.
A medical treatment for life threatening arrhythmias, such as ventricular fibrillation, where cardiac cells randomly fire, resulting in no coordinated ventricular contraction. Defibrillation sends an electric shock through the heart, depolarizing all cells at once, with the hope that the SA node resumes its role as the normal pacemaker. Defibrillation can be done externally to the chest, and internal defibrillators can be implanted as part of a pacemaker.
Pain or cramping in the legs during physical activity. The pain usually resolves with rest. Most often this pain is due to peripheral artery disease and is caused by local ischemia and the accumulation of lactic acid.
The percentage of blood ejected from the left ventricle relative to the end diastolic volume. It is a key measure of heart contraction strength. EF= (stroke volume/ EDV) x 100
Metabolic Equivalent (MET) is an index used to represent the metabolic cost of am activity. One MET equals 3.5ml/kg/min of oxygen use. Different intensities of activities can be quantified in MET values to help describe the metabolic cost.
A work intensity where oxygen delivery to the myocardium is no longer sufficient and the tissue lacks oxygen. This point can be linked to symptoms (angina0 and signs (angina) and identified by the corresponding rate pressure product associated with the work.
