12 Inpatient Cardiac Rehab: Phase I
Program Goals and Exercise Prescription Guidelines
The inpatient is a unique individual, with a range of concerns, comorbidities, and symptoms that they present following some type of cardiac event or surgery. The patient might be an obese, diabetic patient who just had coronary artery bypass graft (CABG) surgery, or perhaps a pulmonary (COPD) patient who had a heart valve replaced. The key to recognize is that all patients are unique, and one cannot just use a turnkey approach to treatment. Exercise science professionals must be attuned to identifying the signs and symptoms that cue them in to the status of a patient. During the 3-5 days after a surgery or event, it is crucial to help the patient become stable and ready to go home. Exercise training in this context is different than traditional exercise environments because the patient is recovering from a serious event.
What are “Signs” and “Symptoms” ?
You have probably heard these two terms used quite a bit, but are you aware of what they are? Let’s separate these terms and look at some examples.
Signs– these represent things that can be measured or identified on the body. For example, blood pressure is not something you necessarily feel, so how do we identify it? We measure blood pressure. A chronic value above 120/80 is a sign indicating hypertension. If your body temperature is above 100-degree F (37 degrees C) what is that a sign of? Fever, right? So, for each patient’s unique condition, there will be key signs that we measure and monitor to indicate their status.
Symptoms– If someone is sweating profusely, what could this mean? Well maybe they have a stomach virus and are going to vomit. Maybe it is a symptom of a myocardial infarction. Maybe they are very anxious? We need more information (perhaps some signs) to be sure. But the patient is displaying symptoms. Symptoms may be reported by the patient (“my chest hurts”) or you might notice the symptoms displayed by observing them (patient began to walk with an uneven gait, with the left side losing control). Exercise science professionals need to have a keen awareness and communication with patients to both observe any patient symptoms and listen to the patient in case they report any symptoms.
| Signs | Symptoms | Condition |
| · ST segment elevation
· Positive test for Troponin I · Positive test for CK-MB |
· Diaphoretic (profuse sweating)
· Pallor (pale) · Chest pain, jaw pain, shoulder, arm pain · Shortness of breath |
Acute Myocardial Infarction |
|
· Reduce Oxygen Saturation (under 92%) · Positive chest x-ray showing edema · Weight gain (fluid retention) |
· Shortness of breath (dyspnea) · Dizziness · Pallor (pale) · Fatigue |
Pulmonary Edema in a heart failure patient |
|
· ST segment depression · Measured rate pressure product that is linked to ischemia inducing work
|
· Angina (pain) in chest, jaw, arm · Dyspnea · Fatigue |
Ischemia in cardiac patient |
|
· Ankle-brachial index measured below 90
· Reduce peripheral blood flow measured with doppler |
· Leg pain upon exertion, resolves with rest
· Pain seems limb specific |
Ischemia in peripheral artery disease patient |
|
· Measured blood sugar below 70 mg/dl (mild) below 54mg/dl (moderate) |
· Shakiness · Dizziness · Confusion · Fatigue · Difficulty speaking |
Hypoglycemic (Diabetic?) patient |
When you have a new inpatient, learn about the patient! Study their case, understand the different conditions they present with, and surgical wounds to monitor as well as signs and symptoms linked to their condition. Be present- pay attention.
Inpatient Cardiac Rehab- Phase I Goals
These days, patients are moved from inpatient to being sent home quickly. For most cardiac patients, they may only be in Phase I (inpatient) for 3-5 days. That is only a short amount of time to address all of the areas needed, but it is an important first step in their (hopefully) lifelong commitment to changing their lifestyle and reducing their risk of another event.
One key point regarding the Phase I patient. Implementing the goals happens when the patient is stable. If there are complications related to their event or recovery, that must first be addressed before implementing the plan. The patient may be in rough shape, but if they are stable, then your work begins!
Goal- Assessment
The exercise science professional should make note of the patient’s condition (diagnosis), their status (stable?), all other comorbidities (overweight? Diabetic?) as well as any reported symptoms (sternal pain, angina pain?). You are also trying to assess whether they are ready to being mobilization (supine to sitting to standing to walking).
According to the American Association of Cardiovascular and Pulmonary Rehabilitation, key factors that suggest they are ready for activity include:
- No new or recurring chest pain in the past 8 hours
- Stable of falling CK-MB and Troponin values
- No indication of decompensated heart failure (dyspnea and low O2 sat at rest, lungs clear)
- Normal cardiac rhythm (stable for past 8 hours)
Get to know the patient according to their medical record, signs and symptoms!
Goal – Mobilization
Bed rest kills! The more the patient is in bed rest the more muscles atrophy, balance and changing body positions (supine to standing) become challenging. The risk of blood clots is always there with bed rest, so getting the patient up and moving is an essential part of phase 1.
Orthostatic Tolerance– a big component of training. It cannot be emphasized enough that a patient passing out and falling could be a very dangerous situation. Most of us take for granted the ability to move from sitting to standing, or simply standing after exercise. However, inpatients often lose orthostatic tolerance, and when they stand up their blood pressure drops (orthostatic hypotension) without the normal baroreflex compensation. They pass out and fall! So never take your eyes off the patient, especially when they transition from supine, to sitting and sitting to standing!
The good news is, with time and exposure, their orthostatic tolerance will come back. So, consider the supine, to sit, to stand and repeat as part of the exercise session. You are helping reestablish their control of blood pressure when changing positions.
Most of the mobilization activities in Phase I are a combination of walking, orthostatic tolerance training and activities of daily living (ADLs).
Walking guidelines (see ACSM Guidelines)
Intensity– Using the seated or standing resting heart rate, limit the patient to an intensity of up to 20 beats above rest for MI patients, and 30 beats above rest for non-MI patients recovering from CABG surgery. An RPE less than or equal to 13 (somewhat hard) can also be used.
Frequency– Two to four session per day during the first 3 days of inpatient
Time– As tolerated! Usually 3-5 minute bouts. The patients may need to rest or slow down. Work with them based on their response! The goal to work for is a 2:1 exercise/rest ratio, where the patient works up to 10-15 minutes of walking with 5 minutes of rest. Each patient will progress differently, so be attuned to the patient.
Vital sign monitoring– Measure heart rate, blood pressure and RPE at each rest opportunity. If systolic pressure begins to drop (>10mmHg) despite increasing workrate, stop exercise. Monitor ECG for any changes in rhythm (atrial ventricular arrhythmias, heart block).
Symptom monitoring– Pain at site of surgery, angina, dizziness, gait changes, pallor complexion, dyspnea. Patients that are stable may move slowly but monitor their symptoms for anything that suggests they are no longer stable.
Goal- Education
Keep in mind that most individuals do not have much understanding on the atherosclerosis process and the risk factors that contribute to it, so helping them understand their disease and how risk factors contribute is important as you help them make a plan moving forward. Some areas to address include:
Risk factors– Hyperlipidemia (HDLs, LDLs contributors), Tobacco use (smoking, chew, marijuana), physical inactivity, hypertension, diabetes control, obesity,
Nutrition– understanding the impact of high sodium diets on blood pressure, heart failure symptoms. Introducing diet information such as the DASH diet, Mediterranean Diet, Pritikin Plan
Medications– Understanding what each drug is being taken for, risks associated with suddenly stopping a medication, side effects and how one might reduce medication use by following nutrition and exercise plans.
Wound Healing– the patient may have sternal incision, radial artery incisions, and leg incisions for saphenous vein removal. Teach the patient how to use a pillow over the sternum when coughing to minimize chest pain at the surgical site.
Part of the education process will be helping them see the broader picture of their risk profile, so that moving forward they can begin a lifestyle designed to reduce the progression of their disease.
Goal Home Care Activities and Recommendations
Just like patients train their system by walking, they also need training in daily care activities. Initially, activities to learn as part of self-care include (with MET equivalents):
Bathing sitting (1.5 Mets)
Toileting (2.3 Mets)
Walking (3.5 Mets)
Stair Climbing (3.0-4.0 Mets)
Upper body use (no resistance) (2.5-3.0 Mets)
Home activities that they can perform will depend on their individual condition, so selecting activities should not only be based on Met levels that are tolerable, but also on any surgical limitation as well as any musculoskeletal limitations of the patient.
Use the Compendium of Physical Activities!
Visit this website : https://pacompendium.com The 2024 Compendium of Physical Activities is a database of activities organized by the types of activities and the associated Met values. You can search the various types of activities and select ones that match the patient’s needs. The patient can then see the energy cost of activities and what activities would be off limits.

Goal- Readiness for Discharge and referral to Phase II (outpatient cardiac rehab)
As the patient is coming to the end of their inpatient stay, it is important that they are provided information about the continuation of their recovery by referral to a Phase II-outpatient cardiac rehab program. Some programs automatically refer patients, while others provide information and leave the discussion to the patient and their cardiologist. However, it is important that the patient understands the importance of phase II and the positive effects it has on quality of life, prolonging life, and improving one’s fitness.
Other discharge planning topics include:
- Knowledge of medications and use (i.e. angina symptoms and when to take nitroglycerine)
- Lifting restrictions (Both due to increases in rate pressure product but also surgical wound healing)
- Sexual activity (limitations, minimize work and stress on sternal incisions)
- Driving (restrictions, where to sit to avoid airbag deployment on chest)
- Stair Climbing (avoid using arms to pull!)
- Awareness of signs and symptoms related to their condition, and how to manage them.
- Home exercise plan for the time between completing phase I and starting phase II
Some facilities may perform some type of low-level exercise test, such as a 6-minute walk test (distance a patient walks in 6 minutes) or a low-level Bruce protocol just prior to release. Patients should be keeping exercise intensity below 5 Mets.
| Stage | Speed (mph) | Grade (%) | Mets |
| 1 | 1.7 | 0 | 2.3 |
| 2 | 1.7 | 3 | 3.0 |
| 3 | 1.7 | 5 | 3.5 |
| 4 | 1.7 | 7 | 3.9 |
| 5 | 1.7 | 10 | 4.6 |
Once the patient is released, it can take 2-4 weeks for the paperwork to process and the patient to enter Phase II cardiac rehab. It will be important to emphasize the importance of maintaining a home exercise plan when they get home.
Your Turn- Let’s put this all together! Case Study
The case study below is designed to mimic some of the information you might have while working with a Phase I inpatient. Complete information in the areas prompted. Work with your instructor and student colleagues to discuss the prompts.
——————————————————————————————————–
Your patient is a 62 year old driver for Gordon Foods. He was admitted to the ER complaining of crushing chest pain, diaphoresis and arm pain that occurred while he was unloading a truck. His ECG at time of admit is below.
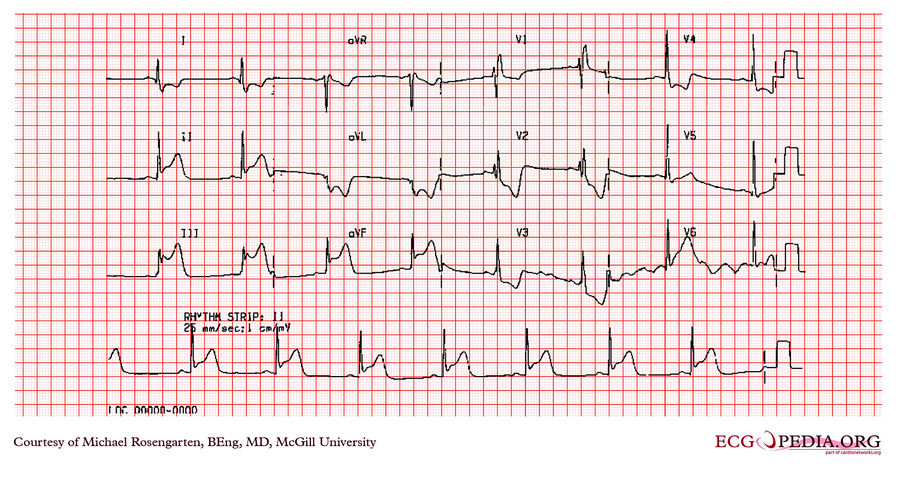
Blood test revealed positive CK-MB and troponin I. Diagnosis was inferior, transmural MI. Patient was treated with morphine, nitroglycerin and heparin. Angiography revealed an 85% occlusion of the LAD and 90% occlusion of the right coronary artery. Ejection fraction via Echocardiography was 50%. Double -bypass CABG was performed using internal mammary artery and saphenous vein. The surgery was successful. Patient discharged to Phase I cardiac rehab. Some residual atelectasis was present, but the patient was otherwise stable.
Time to translate! Define or answer questions below:
- Define “Diaphoresis”- _______________________________________________
- Define Atelectasis____________________________________________________
- What percent occlusion is when blood flow begins to be significantly reduced? 50%, 60%, 70%, 80% circle one
- Which ECG leads are associated with the Inferior aspect of the heart?______________
- What do you see in those leads that is a sign of an acute MI? ___________________
- What other tests help confirm the acute MI __________________________________
- What is a normal resting ejection fraction? 40% 50% 60% 70% circle one
- Why do you think heparin was administered? _________________________________
Phase I Exercise Sessions
Phase I day 1
Rest Hr- 107bpm rest BP- 136/86 Pedal pulse- present
Patient complains of chest discomfort around incision and pain in left leg.
Walking results (snapshot)
Day 1 50 yards HR- 118 BP 160/86 Calculate Rate Pressure Product_________
RPE -14 Patient complains of dyspnea, some chest discomfort, stopped exercise
Day 2 80 yards HR 120 BP 152/86 Rate Pressure product___________
RPE 13 Leg discomfort, ROM activities well tolerated
Day 3 120 yards HR 125 BP 155/84 Rate Pressure product___________
RPE 12 Pace was faster, leg discomfort, ROM well tolerated
- What is the heart rate limit you would use for this patient? ____________________
- What is the RPE limit you would use for this patient? ________________
- What does “ROM” mean? __________________________
Here is a rhythm recorded during one of the walking sessions. Can you interpret it?

- Interpretation __________________________
- Why might the patient be complaining of pain in the left leg while walking? _____________________________________________________________________
- Why did you suggest the patient keep a pillow nearby in case of coughing? _____________________________________________________________________

Using the compendium ( https://pacompendium.com ) and looking under Home Activities and Self-Care, find 6 activities that this patient can complete, while minimizing arm movement and also staying below 5 Mets
| 1._________________________ | 2.______________________ | 3._______________________ |
| 4.________________________ | 5. ______________________ | 6. _______________________ |
Selected Sources
- ACSM Guidelines for Exercise testing and Prescription. 11th ed. Wolters Kluwer Pub. 2022
- Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 5th ed. American Association of Cardiovascular and Pulmonary Rehabilitation. Human Kinetics Pub. 2013
- Matos Casano HA, Anjum F. Six-Minute Walk Test. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK576420/
- Conger S. et al. 2024 Wheelchair Compendium of Physical Activities: An update of activity codes and energy expenditure values. J. Sport & Health Science. 13, 18-23, 2024.
Signs represent things that can be measured or identified on the body, such as blood pressure, body temperature, and oxygen saturation.
Symptoms may be reported by the patient (“my chest hurts”) or you might notice the symptoms displayed by observing them (patient began to walk with an uneven gait, with the left side losing control).
Contractile protein. “I” form located in the heart. When it is found in the blood it is a marker for an acute myocardial infarction
Creatine Kinase-Myocardial Band is an enzyme within heart tissue. During a myocardial infarction, damaged cardiac tissue releases CK-MB into the blood, where it can be measured as evidence of an acute myocardial infarction. It is used as a blood marker of MI.
Difficulty breathing characterized by breathlessness and a feeling of not being able to get enough air in the lungs to relieve the distress. Causes can include COPD, anxiety, deconditioning, and edema caused by heart failure.
Inadequate blood (and therefore oxygen) supply to a tissue. A narrowed or blocked coronary artery results in reduced blood flow to an area of the heart, resulting in reduced oxygen availability.
Relaxed position where the patient lies flat on their back, arms at their side.
Contractile protein. “I” form located in the heart. When it is found in the blood it is a marker for an acute myocardial infarction
A sudden drop in blood pressure when someone moves from supine or seated to standing. This is often accompanied by symptoms of dizziness, pallor complexion and possibly fainting.
A symptom related to heart disease. Characterized by pain in the chest, jaw, shoulder or back. The pain is a result of a lack of oxygen delivered to the heart. It can be transient from a mismatch in oxygen demand and supply to the heart or occur during a myocardial infarction.
Abnormal whitening or pale complexion or tissue bed. It can be a symptom of reduced blood flow to an area.
Metabolic Equivalent. A term used to describe metabolism and oxygen consumption by a huma. I MET equals 3.5 ml/kg/min of oxygen use. The cost of activities can be quantified by how many METs is required to perform the activity or exercise intensity.
Excessive sweating, beyond what is a normal response to the environment. Non exercise reasons for diaphoresis may be anxiety, stress, adverse reaction to medication, myocardial infarction, and fever.
“Across the wall”. In the myocardial muscle this means across the entire width of the myocardial wall
Angiography is a medical imaging technique used to visualize blood vessels in the body, such as arteries and veins. It involves the injection of a contrast agent, usually iodine-based, into the bloodstream to make the blood vessels visible on X-ray images or other imaging modalities like CT scans or MRI scans.
Refers to the complete blockage of a blood vessel or other tubular structure. Sometimes coronary artery degree of blockage is referred to as a percent occlusion. Sometimes used synonymously with the term “Stenosis.”
The percentage of blood ejected from the left ventricle relative to the end diastolic volume. It is a key measure of heart contraction strength. EF= (stroke volume/ EDV) x 100
The collapse or incomplete expansion of the lungs. This is a common occurrence for open heart surgery patients who were on a heart-lung bypass machine. Their lungs had collapsed and have yet to fully recover. Clinicians often have patients cough or “huff” to help create back pressure to help inflate the lungs. Exercise is also used.
