11 Medications Commonly Used in Cardiac Rehab
Each cardiac patient the exercise science professional works with is a different case. They have varied risk factor profiles and present different types of cardiac (and other) concerns. Medications to help address patient symptoms and risks are also varied, however there is a group of medications somewhat common to most cardiac patients. The intent of this chapter is to present information the concept of pharmacokinetics (what happens to the drug once you take it) as well as the most common classes of drugs. The exercise science professional needs to be able to understand the mechanism of action of a drug to know which system is being impacted, indications and use of the drug to understand why the patient is taking the medications, any side effects that might impact the exercise session and how the medications affect any exercise prescription.
Basics of Pharmacokinetics
Pharmacokinetics is a science that studies what the body does with a drug once it is administered. From the standpoint of a patient taking their medications, it is helpful to understand key aspects of how the body manages the drug. These include: 1. Absorption, 2. Distribution, 3. Metabolism and 4. Excretion. Each patient is different, and if a particular organ is involved with metabolism and excretion of the drug, the health of the organ may dictate how the body manages the drug.
Absorption
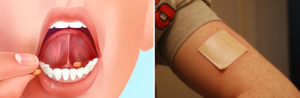
Drugs can enter our system by many different pathways. Most are ingested by mouth, then passing through the digestion, entering the blood stream, and passing through the liver. Other drugs bypass the digestive system altogether and pass directly into the bloods stream. For example, nicotine can be absorbed as a vapor via the lungs (smoking), sublingually (under the tongue) by way of chewing tobacco or even through the dermis in a nicotine patch. Drugs can also be absorbed via intravenous or intramuscular injection.
Once absorbed, not all the drug becomes available to exert its effect. Some drugs availability can be reduced due to food consumed, interaction with other medication, plasma protein binding to the drug rendering it unusable. The term Bioavailability refers to the percentage of a drug that is made readily available for the body. Ingested drugs often have a much lower bioavailability compared to drugs administered intravenously. It is important for the patient to understand the ideal conditions for taking their medication to maximize the absorption and bioavailability of the drug.
Distribution
Distribution refers to how well a drug disperses through the body and is often dependent on how well the patient can move blood (cardiac output) and perfuse tissue. Detrained, and compromised patients may have poor distribution of a drug due to poor circulation and reduced cardiac output. Plasma protein binding can also reduce distribution, since a drug bound to a plasma protein cannot be released into the tissue to exert it effect.
Metabolism
The liver is a vitally important organ for the breakdown of drugs into chemicals that can be excreted. The liver contains a myriad of enzymes that act on chemicals, breaking them down into smaller molecules that are ultimately excreted. Some drugs are metabolized very quickly by the liver, while others take longer. Dosages and timing of medications are often based on the half-life (time for ½ of the drug to be metabolized) of a medication within the system. From a patient perspective, the health of the liver will play a role in their metabolic response to a drug. Some patients may not metabolize a drug at the same rate as expected, so the physician needs to be made aware of any adverse dosing effects, and the exercise science professional should be attentive to patient symptoms or complaints related to medications, so that they can communicate with appropriate health professionals.
Excretion
Excretion or elimination of a drug is the removal of the drug or metabolite of the drug from the body. Chemicals may be eliminated via respiration, sweat, saliva, tears and even breast milk. However, the bulk of elimination is via the kidneys. The kidneys filter all blood and secrete wastes, including drug metabolites for urinary excretion. For the patient, the ability to effectively excrete the drug is again somewhat dependent upon the health of the kidney, so one cannot assume a predictable excretion rate of a medication. Communication between the patient and the health care provider is essential to fully understand the complete absorption to excretion cycle of medications in each patient, and in some cases medication changes may be warranted.
Mechanism of Action: How does the drug exert its effect?
When a patient takes a medication, there is an interaction of the drug with their physiology. The drug will exert an effect by binding to a receptor, blocking some type of enzymatic reaction, or perhaps preventing the movement of other chemicals into cells. Mechanism of action refers to the description of how the drug exerts its effect on the body. It may do this by interacting with a specific organ or tissue.
Indication and Use: What is the drug being used to treat?
Drugs can often exert more than one effect, but often they are created for a specific condition “Indication” refers to the valid or accepted reason to take the drug. Perhaps the drug is used to lower blood pressure, lower cholesterol, or some other desired effect for the patient. In some cases, the drug may also be used for other, less common situations. For example, you will see that beta blockers are used quite often to ease the work of the heart in heart disease patients but is sometimes also used to treat migraines on non-heart disease patients.
Side effects: unintended effects
Unfortunately, drugs often are less precise than we would like them to be. The physiology of the human body is complicated. For example, you might want to block histamine receptors in the tissue to stop an allergic reaction, but histamine receptors are also blocked in the brain. In the brain, histamine is related to our state of arousal, or awakeness, so blocking them makes us sleepy. This is not a desired outcome but is rather a side effect of the drug. Side effects might be common or appear infrequently. Or perhaps if the patient has compromised organs (liver, kidney) side effects might be more prevalent. So do not think of side effects like they WILL happen, but rather that they are possible. The patient should be made aware of potential side effects, be monitored to see if they manifest, and then work with the physician for alternative treatments if the side effects are problematic.
Effects on exercise
For the exercise science professional, it is important to determine if the medication will alter variables that are used within an exercise prescription. Most often, we monitor heart rate and blood pressure since they are key indicators of the work (myocardial oxygen use) of the heart. If a drug lowers blood pressure, then it is easing the work of the heart and may allow the patient to exercise at a higher intensity without symptoms. We should always examine the medications a patient is taking to see any drug related impacts on the exercise plan.
Drug Classes
Drugs may be classified according to the indications and uses (i.e. anti-hypertensive drugs) or according to the mechanism of how they act. That is how this section is organized. It is impossible to memorize every drug that a patient might take. However, drugs that are grouped into their same mechanism of action are going to act very similar. Therefore, if you can at least remember how the drug class exerts its effect, then you will have a good sense of what the drug does, even if all you know is the classification. Let’s look key drugs that are used often with cardiac rehab patients. This list is not inclusive of all drugs used, but with an understanding of how these drugs work, you better equipped when investigating a new medication unfamiliar to you.
Beta Blockers (beta antagonists)
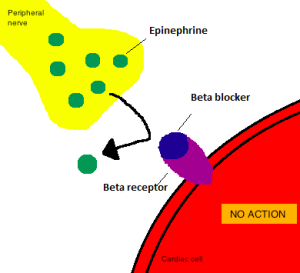
Beta receptors are located throughout the body, and there are several slightly different subtypes of beta receptors. The receptors most common to the heart, blood vessels and lungs are Beta 1 (heart, blood vessels) and beta 2 (bronchioles). Epinephrine is a beta agonist, so when “Epi” is released into the blood it binds with these receptors. The agonistic effect is an increase in heart rate and blood pressure (beta1) and bronchodilation (beta 2). This is the fight or flight response and prepares the body for exercise. For the cardiac patient, lowering heart rate and blood pressure is an important part of easing work of the heart, so beta blockers are very common drugs.
Mechanism of Action- Non-selective Beta blockers compete with epinephrine for the beta 1(heart and blood vessels) and beta2 receptor (bronchioles), and when the dose of the drug is high enough, beta blockers bind to beta receptors and block the action of epinephrine, lowering heart rate and blood pressure. Selective beta blockers only affect beta 1 receptors.
Indications and Use: This drug is used for the management of hypertension, angina, heart failure and fast rate arrhythmias (“tachyarrhythmias”). It is also used for the treatment of migraines and some types of tremors.
Side effects: may block signs of low blood sugar in diabetic patients, bronchospasm, fatigue, dizziness, erectile dysfunction, anxiety, depression
Precaution with bronchioles– Beta 2 receptors affect bronchodilation, so blocking these receptors can cause bronchoconstriction in patients with bronchiole conditions (asthma). In those instances, a beta 1 selective beta blocker is indicated.
Effects on exercise: This class of drugs lowers both heart rate and blood pressure. It therefore also lowers rate pressure product (HR x systolic BP).
In cardiac patients– This reduced oxygen use by the heart and may relieve anginal symptoms. By lowering RPP, it may allow the individual to exercise at a higher intensity before they reach a point of angina.
In non-cardiac patients– For non-cardiac patients taking beta blockers for migraines, there is a lowering of heart rate, which lowers peak cardiac output (HR x SV). Therefore, they will notice a reduced work capacity. For athletes or exercisers, they may consider alternative migraine treatments that won’t lower their heart rate.
Table 1. List of Selective (beta 1) and non-selective (beta 1&2) beta blockers
| Selective
Generic (Brand) |
Non-selective Generic (Brand) |
| Metoprolol (Lopressor) | Propanolol (Inderol) |
| Acebutolol (Sectral) | Timolol (Blocadren) |
| Atenolol (Tenormin) | Nadolol (Corgard) |
| Esmolol (Brevibloc) | Sotalol (Betapace) |
| Bextaxolol (Kerlone) | Carvedilol (Coreg) |
| Celiprolol (Selectol) | Labetalol (Trandate) |
Calcium Channel Blockers
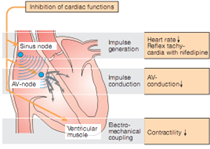
During the excitation of cardiac cells there is an inward current of calcium involved in the depolarization of the cell. Additionally, calcium is used in smooth muscle to contract (vasoconstrict). Calcium is also involved in assisting the propagation of signals through the AV node. Therefore, calcium channel blockers inhibit the inward flow of calcium, and reduce the actions in cardiac cell depolarization, AV node conduction and blood vessel constriction. There are three different types of calcium channel blockers, and they impact the heart and blood vessels differently.
Mechanism of Action: Due to differences in different types of calcium channel blockers, there are variations in the mechanism of action and effects.
Three CA blocker variants exist:
- Verapamil– Large effect on AV node blockage (i.e slowing impulses through AV node in cases of Afib, SVT, Aflutter). Mild effect on vasodilation. Negative inotrope.
- Nifedipine– Large effect on vasodilation (effective to lower blood pressure). No inotropic effects, no AV node effects.
- Diltiazam– Some vasodilation, some reduction in inotropy and some AV blockade.
Indications and Use: From the information previous, one can see that indications and use depend on the medication. For example, if treatment of hypertension is indicated, then Nifedipine would be the drug of choice. Nifedipine is also indicated for angina treatment, as well as coronary vasospasm.
For treatment of Atrial fibrillation and reducing ventricular response rate, Verapamil is indicated. So primary indication and use of this drug is to treat supraventricular arrhythmias. It is also used to treat hypertension.
Diltiazem, due to its wider range of effects is used to treat angina, hypertension as well as supraventricular arrhythmias.
Side effects: hypotension, bradycardia, dizziness, flushing, fatigue, headaches, edema, AV block
Effects on exercise: Effects on exercise may vary, depending on the drug being administered. Most will see a reduction in blood pressure and therefore rate pressure product. Patients with supraventricular arrhythmias may see a reduced ventricular response rate and therefore a lower heart rate.
Table 2. CA Channel Blockers
| Dihydropyridine-type
Generic (Brand) |
Phenylalkylamine–typeGeneric (Brand) |
Non-dihydropyridine-type
Generic (Brand) |
| Nifedipine (Procardia) | Verapamil (Calan, Isoptin) | Diltiazem (Cardizem) |
| Amlodipine (Norvasc) | Gallopamil | |
| Barnidipine (HypoCa) | Fendiline | |
| Lacidipine (Motens) |
Nitrates-Nitroglycerine
Within smooth muscle, there is a gas that forms called nitric oxide (NO). Precursors for NO come from foods, especially rooted plants (nitrates). Nitric oxide is a blood vessel dilator, but only appears for a short time once created. The drug Nitroglycerin was discovered in the late 1800’s and found to be a potent vasodilator. It is now known that it is an exogenous supply of nitric oxide and can cause rapid onset vasodilation, particularly on the venous side.
Work of the heart: Preload vs Afterload
If you can picture standing in a line and passing sandbags to toss onto a truck, you might be able to imagine the concept of “Preload” and “Afterload”. Imagine a 100 pound sandbag that gets handed to you coming from the line (this is preload). Next you are expected to toss that bag up onto a truck (this is afterload). Both preload and afterload create a lot of work! Preload in the cardiac sense is venous return, or the volume of blood coming back to the heart and filling the ventricle. High venous return creates a heavier load for the heart to push. Afterload is the systemic pressure (blood pressure) that the ventricle must push against to eject blood from the ventricle. Lowering either one (or both) of these variables reduced the work of the heart. It’s like giving you a 50- pound sandbag instead, or lowering the size of the toss!
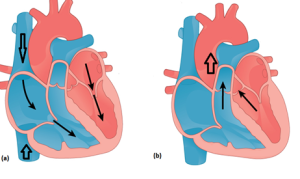
Nitroglycerin Mechanism of Action
Nitroglycerine acts as a strong venous blood vessel dilator as well as an arterial system dilator (not as potent). It is thought that the drug acts as a supply of exogenous nitric oxide, causing vasodilation, resulting in reduced venous return and lowered blood pressure.
Indications and Use
Nitroglycerin is used for the treatment of anginal attacks by reducing the workload on the heart and help prevent anginal attacks from becoming worse.
Side effects– Track the patient’s blood pressure when they take nitro! Nitroglycerine can cause side effects related to dropping the blood pressure too much. These include dizziness, headache, and hypotension. In some cases, the drop in blood pressure triggers reflex tachycardia. Patients using other vasodilators, such as erectile dysfunction drugs should not combine with nitro, as this may result in significant blood pressure drops.
Effect on exercise– In patients with chronic angina, nitroglycerin can reduce the load on the heart at a given workrate by reducing blood pressure and venous return. This means that the patient may be able to do more work (higher MET training) without incurring the same cardiac load. This allows for a better training program and outcome. Nitroglycerine can also be effective in circumstances where exercise induced anginal symptoms that do not resolve by rest alone.
Table 3. Brand Names of Nitroglycerine
| Gonitro | Nitrocot | Nitrolingual | NitroMist |
| Nitroquick | Nitrostat | Nitrotab | Nitro-Time |
Angiotensin Converting Enzyme Inhibitors (ACE inhibitors) and Angiotensin Receptor Blockers
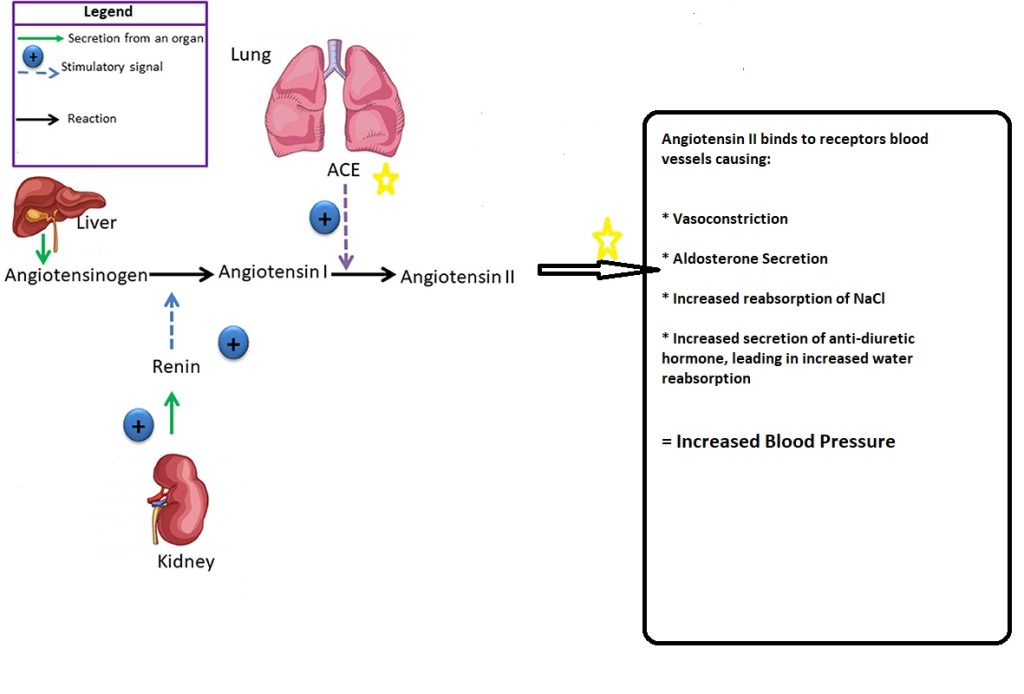
High blood pressure is a significant strain on the heart, and there are a range of reasons why blood pressure is elevated. One area involves the liver and kidneys and the signals and controls for regulating blood pressure. The Renin-Angiotensin system helps regulate blood pressure and electrolyte balance in the blood. If renal (kidney) blood flow is low, signals to increase blood pressure come in the form of Renin, released by the kidneys. Renin interacts with angiotensinogen, released by the liver to form Angiotensin I.
By itself Angiotensin I is benign and has no effect. However, when passing through the lungs it interacts with an Angiotensin Converting Enzyme (ACE). ACE converts Angiotensin I into Angiotensin II, which then binds to receptors on blood vessels to cause vasoconstriction and increased blood pressure.
ACE Inhibitors
Mechanism of Action: ACE inhibitors block the conversion of angiotensin I into angiotensin II. They also lower aldosterone levels. The net result is systemic vasodilation.
Indications and Use: Lowering blood pressure in hypertensive patients. Improving symptoms of patients with heart failure.
Side Effects: Dizziness, drowsiness, fatigue, headache, cough, hypotension, taste disturbances.
Effect on Exercise: Reducing blood pressure lowers rate pressure product (HRx SBP) which reduces the workload on the heart. This can allow the angina patient to do more physical work without symptoms.
Table 4. ACE inhibitors- Generic(Brand)
| Lisinopril (Zestril) | Enalapril (Vasotec) | Quinapril (Accupril) | Captopril (Capoten) |
| Moexipril (Univasc) | Trandolapril (Mavik) | Benazepril(Lotensin) | Ramipril (Altace) |
Angiotensin Receptor Blockers
Mechanism of Action: Blocks vasoconstrictor and aldosterone producing effects of angiotensin II at receptor sites in vascular smooth muscle and adrenal glands
Indications and Use: treatment of hypertension. Decreasing progression of heart failure, lowering heart failure symptoms
Side Effects: Dizziness, drowsiness, fatigue, headache, cough, hypotension, taste disturbances.
Effect on Exercise: Reducing blood pressure lowers rate pressure product (HRx SBP) which reduces the workload on the heart. This can allow the angina patient to do more physical work without symptoms.
Table 5. Angiotensin Receptor Blocker- Generic(Brand)
| Losartan(Cozaar) | Valsartan (Diovan) | Olmesartan (Benicar) | Azilsartan (Edarbi) |
| Telmisartan(Micardis) | Irbesartan (Avapro) | Candesartan (Atacand) | Eprosartan (Teveten) |
Diuretics
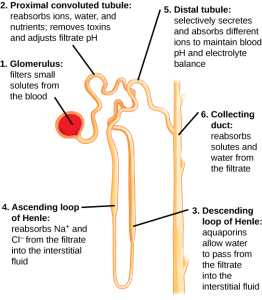
The kidney is the organ primarily responsible for filtering our blood and eliminating fluid in the form of urine. All blood is filtered through the glomerulus, which is part of each nephron (smallest functional unit of the kidney. From there nutrients can either be reabsorbed back into the blood or secreted and eliminated in the urine. Long term blood volume and blood pressure control is an essential part of the kidneys function.
As fluid passes along the different aspects of the nephron, solutes such as sodium, potassium, chloride, glucose along with water are reabsorbed or secreted. Different parts of the nephron absorb differently. For example, the descending loop of Henle is highly permeable to water reabsorption back into the blood, while the ascending loop is not permeable to water, but instead is where ion exchange happens.
Diuretics, or as lay people often call then “water pills” are designed to affect different aspects of the nephron to manage ion exchange and water transport, with the goal most often being to reduce blood volume by reducing water reabsorption. As a result, there are several different types of diuretics according to their functional site of action.
Distal Convoluted Tubule Diuretics- Thiazide Diuretics
Mechanism of action: Thiazides inhibit the reabsorption of sodium from the distal convoluted tubule. This promotes a reduction in plasma sodium as well as a reduction in water reabsorption (diuresis) and a reduction in blood volume.
Indications and Use: Management of hypertension. These drugs are used often alone or in conjunction with other antihypertensive drugs to help reduce blood pressure. It is also used to reduce edema associated with congestive heart failure.
Side effects: Most side effects are a result of an imbalance caused by ion and sodium loss. This includes low potassium (hypokalemia), low sodium (hyponatremia, high calcium (hypercalcemia), high glucose (hyperglycemia).
Effects on Exercise: Reductions in blood pressure will reduce rate pressure product (HRx SBP) and therefore the patient may be able to exercise at a higher work intensity without elevating RPP to ischemic levels.
Table 6. Thiazide Diuretics- Generic (Brand)
| Hydrochlorothiazide (Microzide) | Chlorthiazide (Diuril) | Indapamide (Lozol) | Metolazone (Zaroxolyn) |
Loop-Acting Diuretics
Mechanism of action: Inhibits the reabsorption of NaCL in the loop of Henle, resulting in large volume water excretion. Also inhibits potassium, calcium and magnesium reabsorption.
Indications and Use: Management of hypertension. Used to treat edema associated with congestive heart failure. First-line treatment for heart failure due to reduced ejection fraction and volume overload
Side effects: hypokalemia, hyponatremia, hypochloremia, hypomagnesemia, hyperuricemia, gout, headache, dizziness, postural hypotension
Effects on Exercise: Reductions in blood pressure will reduce rate pressure product (HR x SBP) and therefore the patient may be able to exercise at a higher work intensity without elevating RPP to ischemic levels. In heart failure patients, reduced edema may reduce symptoms of dyspnea and low oxygen saturation, making exercise more tolerable.
Table 7. Loop-acting Diuretics- Generic (Brand)
| Furosemide (Lasix) | Bumetanide (Bumex) | Torsemide (Demadex) | Ethacrynic acid (Edecrin) |
K+ Sparing Diuretics
As seen previously with thiazide and loop acting diuretics, the loss of potassium can be substantial. As the name implies, K+-sparing diuretics have a diuretic effect but do not cause potassium loss.
Mechanism of action: Acts to prevent sodium reabsorption in the collecting tubule of the nephron by blocking sodium channels or aldosterone receptors (depending on the drug). This prevents the excretion of K+ and mild diuresis.
Indications and Use: Used as an adjunct in the management of hypertension, cirrhosis, and congestive heart failure.
Side effects: High potassium levels (especially if taken with ACE inhibitors), dizziness, breast tenderness or swelling, nausea, weakness, irregular heart beats.
Effects on Exercise: Lowers blood pressure (mild) without causing potassium loss. In heart failure patients can help reduce blood pressure and reduce potassium loss.
Table 8. K+-sparing Diuretics Generic (Brand)
| Spironolactone (Aldactone) | Triemterine (Dyrenium) | Amiloride (Midamore) | Eplerenone (Inspsra) |
Cardiac Glycosides
Cardiac glycosides are chemicals in nature. Plants (i.e common foxglove) produce the chemical as an evolutionary strategy to reduce predation (makes them less palatable). Some insects consume these plants and concentrate the chemical in their cells as a deterrent (i.e Monarch butterfly). However these chemicals bind to the Na,K-ATPase pump, which regulates ion flow into and out of cells to maintain proper concentrations of ions in and out of the cell. Therefore, in small amounts it can affect ion concentrations and therefore depolarization of cardiac cells.
Mechanism of Action: Acts on the cardiac myocyte to inhibit the Na+/K+-ATPase pump, resulting in an accumulation of NA+ within the cell. This allows the NA+/CA+ exchange channel to bring more calcium into the cell, thereby causing a stronger muscle contraction (positive inotropic effect). Glycoside also increases the refractory time within the AV node.
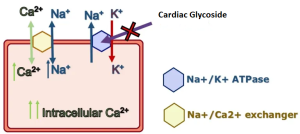
Indications and Use: Used as a positive inotropic agent in the treatment of congestive heart failure. Also used in treatment of supraventricular arrhythmias (SVT, atrial fibrillation) where a lengthening of AV node refractory period is desired.
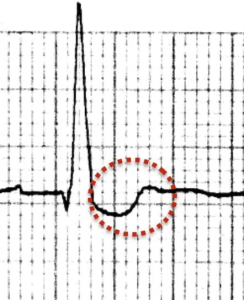
Side effects: Toxicity. The therapeutic window is narrow for cardiac glycosides, and toxicity is a potential side effect, which can lead to vomiting, loss of vision, confusion, irregular heart rate and even death. Common ECG changes include a “scooped” ST segment.
Effects on Exercise: Cardiac glycosides like digoxin are positive inotropes. These will increase ejection fraction for patients with reduced EF (i.e. heart failure). For patients with atrial fibrillation, it may reduce the ventricular response rate by slowing the number of signals getting through the AV node, resulting in lower resting and exercise heart rates.
Table 9. Cardiac Glycosides – Generic (Brand)
| Digoxin, Digitalis (Digitek) (Digox) (Lanoxin) |
Anticoagulant and Antiplatelet Drugs
For patients with atrial fibrillation of circulatory problems like peripheral vascular disease, deep vein thrombosis or ischemic stroke, blood clots are common and potentially lethal occurrence. Drugs to prevent the initial clot formation of platelet adherence or actual clot formation is the purpose of the antiplatelet and anticoagulant drugs.
Anticoagulants
Anticoagulants are types of medications that interfere with blood clot formation. Lay people call these drugs “blood thinners” There are different types of anticoagulants that work on different points of the blood coagulation sequence.
Types of Anticoagulants and Mechanism of Action:
Coumarins and Indandiones– Oral drugs that inhibit Vitamin K epoxide reductase, which blocks coagulating factors II,VII, IX and X preventing blood from clotting
Factor Xa inhibitors– Selectively and reversibly block the activity of clotting factor Xa, preventing clot formation. Prevents activation of prothrombin to thrombin.
Heparins– Injectable coagulant that activates antithrombin III, which inhibits thrombin and factor Xa, thereby blocking clot formation.
Thrombin Inhibitors– Bind to thrombin and inhibit the activity of thrombin, preventing blood clot formation. Binds to free thrombin as well as thrombin bound to fibrin.
Indications and Use– anticoagulants are prescribed to treat blood clots and to prevent blood clot formation due to conditions such as atrial flutter/fibrillation, deep vein thromboses, pulmonary embolism, ischemic stroke risk, post-surgery (hip, knee), or MI prevention.
Side effects– The primary side effect is bleeding. Bleeding from a cut that lasts for more than 5 minutes when applying pressure, coughing up blood, severe headache, red or brown urine, unusual bruising, tissue necrosis.
Effects on exercise– be aware of the bleeding risk. Use precaution when prescribing exercise to avoid activity that may result in a bruise (i.e. stationary cycling instead of outdoor cycling). Patients at risk of falling are a particular concern.
Table 10. Anticoagulants – Generic (Brand)
| Coumarins and Indandiones | Factor Xa inhibitors | Heparins | Thrombin Inhibitors |
| Warfarin (Coumadin) | Rivaroxaban (Xarelto) | Enoxaparin (Lovenox) | Dabigatran (Pradaxa) |
| Warfarin (Jantoven) | Apixaban (Eliquis) | Dalteparin (Fragmin) | Bivalirudin (Angiomax) |
| Fondaparinux (Arixtra) | Tinzaparin (Innohep) | Desirudin (Iprivask) |
Antiplatelet Medications
Platelets circulate in an inactive state within the circulatory system but become activated in response to endothelial damage, such as atherosclerotic plaque rupture. Platelet activating factors, such as thrombin and collagen are released into circulation, initiating the platelet activation pathway. The result is platelet binding to damaged cells to reduce bleeding. However, in atherosclerotic plaque rupture the result can be a blood clot that causes a myocardial infarction of stroke. Antiplatelet medications are designed to interrupt the platelet activation pathway.
Types of Antiplatelet Medications and Mechanism of Action:
Aspirin and cyclooxygenase inhibitors– Works to irreversibly inhibit the cyclooxygenase enzyme (COX) activity, which reduces platelet aggregation and causes vasodilation.
Oral thienopryridines– Selectively inhibit ADP-induced platelet aggregation by inhibiting the platelet P2Y12 receptor.
Dipyridamole– Inhibits platelet nucleotide phosphodiesterase, which inhibits platelet aggregation and induces vasodilation.
Indications and Use: Acute ischemic stroke, post CABG surgery, post PCI with stent, atrial fibrillation, venous thromboembolism prevention, mechanical heart valve surgery
Side effects: Upper GI bleeding, hemorrhage, blood in urine, headache, nausea, discoloration of skin from bruising.
Table 11. Antiplatelet Medications – Generic (Brand)
| Cyclooxygenase inhibitors | Oral Thienopryidines | Dipyridamole |
| Acetylsalicylic acid (Aspirin) | Clopidogrel (Plavix) | Dipyridamole (Persantine) |
| Indomethacin (Indocid) | Prasugrel (Effient) | |
| Ibuprofen (Advil, Motrin) | Ticlopidine (Ticlid) |
Cholesterol Lowering Drugs- anti-hyperlipidemics
Cholesterol is a substance synthesized in humans and is an important component of cell membrane structure. It is also a foundational molecule for the formation of Vitamin D, steroid hormones, and sex hormones (estrogen, testosterone, progesterone). So, we need it! The liver is the organ responsible for the creation and recycling of cholesterol in the body. Since cholesterol is a lipid (it can’t dissolve in the blood plasma), it must be carried. The liver wraps cholesterol in proteins. The two cholesterol-protein wrapped molecules (called “lipoproteins”) of heart disease interest are LDL and HDL cholesterol. HDL cholesterol is a molecule that can take cholesterol from cell membrane for removal and is often referred to as the “good” cholesterol, while LDL cholesterol (“bad cholesterol”) deposits cholesterol, and in an oxidized for can both damage arterial walls and deposit cholesterol, contributing to atherosclerosis. Cholesterol lowering medications typically are designed to lower overall circulating cholesterol, lower LDL-C and increase HDL-C.
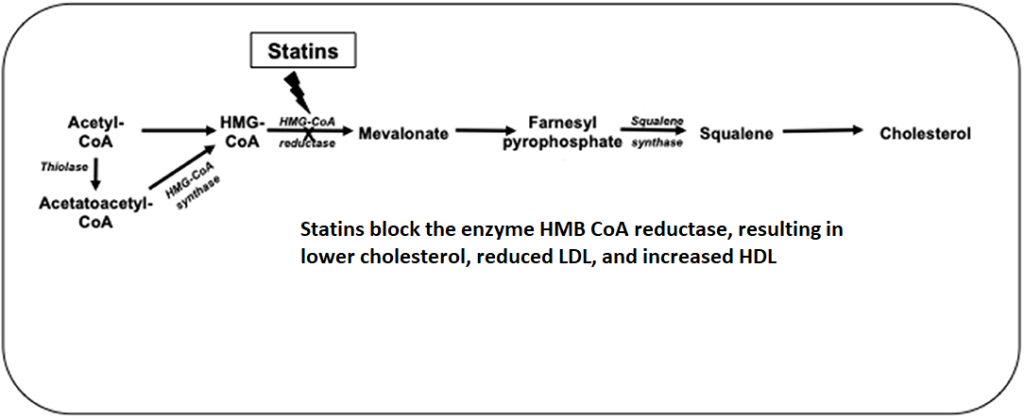
Statins
Mechanism of Action: Statins block the enzyme HMB-CoA reductase, which is an important step in cholesterol synthesis. As a result, circulating cholesterol and LDL-C is lowered, with some increase in HDL-C.
Indication and Use: Statins are used in both primary and secondary prevention of heart disease. They are indicated in cases of elevated cholesterol or LDL-C.
Side effects: Muscle pain is a somewhat common side effect that should be monitored, increase in some liver enzymes is also possible, so blood tests should occur on an annual basis.
Effect on Exercise: Statins have no effect on heart rate or blood pressure. Monitoring muscle pain associated with exercise is prudent, given the potential side effects associated with statin therapy.
Table 12. Statin Medications – Generic (Brand)
| Rosuvastatin (Crestor) | Atorvastatin (Lipitor) | Simvastatin (Zocor) |
| Lovastatin (Mevacor) | Fluvastatin (Lescol) | Pravastatin (Pravachol) |
Bile Acid Sequestrants
Bile acids are synthesized in the liver. The purpose of bile acids is to assist with the digestion and breakdown of dietary fats and oils. One primary component of bile acids is cholesterol. Normally bile acids are cycled between the liver and the GI tract.
Mechanism of Action: Bile acid sequestrants bind to components of bile acids, preventing them from being reabsorbed from the gut, and instead causing them to be eliminated. This results in a reduction of the cholesterol circulating in the system, and results in a lowering of total cholesterol and LDL cholesterol.
Indications and use: Used for the treatment of hypercholesterolemia.
Side effects: Most side effects are related to the GI tract, such as diarrhea, bloating, flatulence and constipation
Effects on Exercise: None
Table 13. Bile Acid Sequestrants – Generic (Brand)
| Colestipol (Colestid) | Colesevelam (Welchol) | Colestyramine (Questran) |
Fibrates
Mechanism of action: Fibrates, stimulate the metabolism of triglyceride molecules and HDL-C cholesterol. They can result in a reduction in triglycerides by 50% while increasing HDL-C by 20%. LDL changes are less apparent.
Indications and Use: used in the treatment of high triglycerides and low HDL. May be used in combination with statins.
Side effects: stomach upset, muscle pain and damage (increased risk of rhabdomyolysis in patients also taking statins). Increased AST, ALT liver enzymes.
Effects on Exercise: None
Table 14. Fibrates – Generic (Brand)
| Fenofibric acid (Trilipix) | Gemfibrozil (Lopid) | Fenofibrate (Tricor) |
Niacin
Also known as nicotinic acid and vitamin B3, niacin is an essential nutrient in the diet. However doses much higher than RDA dose ranges have been used in the treatment of high cholesterol and LDL-C.
Mechanism of Action: Large doses decrease lipoprotein and triglyceride synthesis by inhibiting the release of free fatty acids from adipose tissue, decreasing hepatic lipoprotein synthesis.
Indications and Use: adjunctive therapy for hypercholestrolemia
Side Effects: Vasodilation effect such as flushing of the skin, itching, dizziness, GI upset hypotension, tingling skin
Effects on Exercise: None
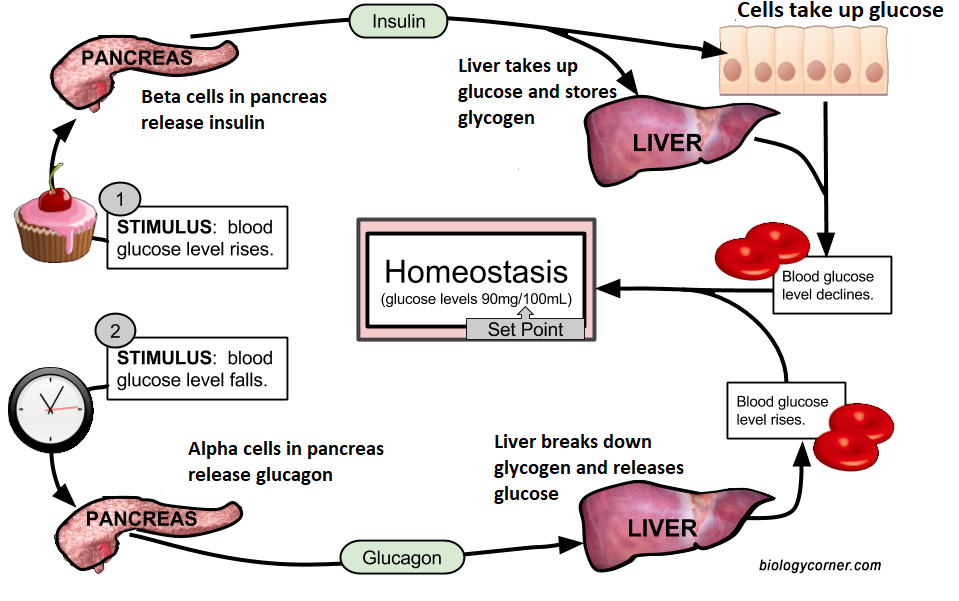
Blood Glucose Mediators
The blood stream is transport system for glucose, either to direct the glucose to storage as glycogen, or to transport glucose to the cells for ATP production. Typically, blood glucose levels are regulated within a range of 70 to 100 mg/ml. Insulin and glucagon, both released by the pancreas, help mediate glucose homeostasis. Type I diabetes is a result of a lack of insulin production by the pancreas, while type II diabetes is an impairment in the sensitivity of insulin receptors to draw glucose out of the blood. Both result in elevated blood glucose levels. Medications to either provide insulin exogenously (for type I) or impact the physiology of glucose metabolism (type II) are used along with diet and exercise to help control blood glucose.
Insulin Medications for Type I Diabetes
Because the type I diabetic does not have the ability to vary the amount of insulin in the blood the way a normal functioning pancreas can do for us, they must rely upon insulin that has varied rates of effect. Fast acting insulin may be good for right after a meal, but longer acting can help normalize glucose throughout the day. So, insulin medication will vary by the nature of the duration of the drug effect.
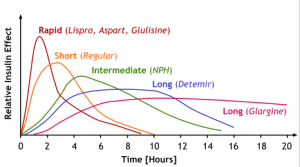
Insulin mechanism of action: Insulin increases the absorption of glucose in muscle and liver, resulting in the lowing of blood glucose. Insulin increases glucose uptake by fat cells as well as fatty acids, resulting in increases in triglyceride storage. It also increases protein synthesis by controlling amino acid uptake. Insulin blocks glycogen, protein and fat breakdown.
Indications and use: Insulin is used to treat type I and type II diabetes.
Side effects: Insulin can draw too much glucose into the cells and cause hypoglycemia, so the dosing and timing of insulin is important.
Effect of exercise: Exercise has an insulin-like effect. This means that exercise also acts to draw glucose into the cell and must be considered when dosing and timing insulin administration. Also consider the site of the drug injection; if you inject into a leg, and then exercise with the leg, insulin may be circulated faster than expected due to increased blood flow. Therefore, the patient should consult with their physician, and perhaps an abdominal injection site would be better.
Medications to Treat Type II Diabetes
Because the diabetic has lost control of glucose metabolism across the spectrum of glucose control, a range of drugs with varied mechanisms of actions are used to try to regain normal glucose levels. They are presented in table form here:
Table 15. Medications to Attain Glycemic Control
| Drug Class | Drug name | Mechanism of Action | Adverse effects |
| Biguanide | Metformin | Insulin sensitizer, inhibits hepatic glucose production | Vitamin B12 deficiency. |
| Dipeptidyl peptidase 4 (DPP-IV) inhibitor | Alogliptin
Sitagliptin Linagliptin Vidagliptin Saxagliptin |
Inhibit the degradation of GLP, resulting in greater insulin release and reduced glucagon. | Pancreatitis, upper RTI (infection) |
| Sodium-glucose cotransporter (SGLT2) inhibitor | Canagliflozin
Dapagliflozin Empagliflozin |
Blocks glucose reabsorption from proximal tubule | Ketoacidosis, genital mycosis (yeast infection), bone fractures |
| GLP-1 agonists | Liraglutide
Exenatide Dulaglutide |
Activates GLP-1 receptor, increases insulin secretion, decrease glucagon | Nausea, vomiting, C cell tumor of thyroid |
| Sulfonylureas | Glimepiride
Glipizide Glyburide |
Increases insulin secretion | Caution use with beta blockers, nausea, weight gain |
| Thiazolidinediones (TZD) | Rosiglitazone
Pioglitazone |
Insulin sensitizer | Bladder cancer, fractures |
Antidepressants
Depression is a common issue with cardiac patients, and use of antidepressants is widespread even among non-cardiac patients. Medications may vary according to the reported symptoms of the patient. Health experts believe that neurotransmitters in the brain influence depression symptoms, notably: serotonin, norepinephrine and dopamine. Most antidepressant medications influence the concentration of these transmitters.
Table 16. Antidepressant Medications
| Drug Class | Drug name | Mechanism of Action | Adverse effects |
| Serotonin Reuptake Inhibitors (SSRIs) | Fluoxetine (Prozac)
Paroxetine (Paxil) Sertraline (Zoloft) Citalopram (Celexa) Escitalopram (Lexapro) |
Inhibits the reuptake of serotonin in the CNS (elevates levels) | Anxiety, drowsiness, headache, insomnia, nervousness, diarrhea, sexual dysfunction |
| Monoamine oxidase inhibitors (MAOIs) | Tranylcypromine (Parnate)
Phenelzine (Nardil) Isocarboxazid (Marplan) |
Inhibits enzyme monoamine oxidase. Increased dopamine, epinephrine, norepinephrine, serotonin | Hypertensive crisis, dizziness, headache
Dangerous interactions with food containing tyramine (cheese, pickles, wines) |
| Tricyclic antidepressants | Imipramine (Tofranil)
Nortriptyline (Pamelor) Desipramine (Norpramin) Doxepin |
Potentiates the effect of serotonin norepinephrine. Anticholinergic properties | Do not use concurrent with MAO inhibitors!
Suicidal thoughts, drowsiness, hallucinations, constipation |
| Serotonin-norepinephrine reuptake inhibitors | Duloxetine (Cymbalta)
Venlafaxine (Effexor) Desveblafaxine (Pristq) Levomilnacipran (Fetzima)
|
Inhibits serotonin and norepinephrine reuptake in CNS. Decreases depressive symptoms, decreased pain, anxiety | Decreased appetite, fatigue, drowsiness, dizziness, nightmares
Do not use concurrent with MAO inhibitors!
|
Selected Sources
Akbari P, Khorasani-Zadeh A. Thiazide Diuretics. [Updated 2023 Jan 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532918/
Chaudhury A, Duvoor C, Reddy Dendi VS, Kraleti S, Chada A, Ravilla R, Marco A, Shekhawat NS, Montales MT, Kuriakose K, Sasapu A, Beebe A, Patil N, Musham CK, Lohani GP and Mirza W (2017) Clinical Review of Antidiabetic Drugs: Implications for Type 2 Diabetes Mellitus Management. Front. Endocrinol. 8:6. doi: 10.3389/fendo.2017.00006
Davis Drug Guide for Nurses: www.drugguide.com
El-Mallakh RS, Brar KS, Yeruva RR. Cardiac Glycosides in Human Physiology and Disease: Update for Entomologists. Insects. 2019 Apr 10;10(4):102. doi: 10.3390/insects10040102. PMID: 30974764; PMCID: PMC6523104.
Front. Cardiovasc. Med., 20 May 2021 Sec. Lipids in Cardiovascular Disease Volume 8 – 2021 | https://doi.org/10.3389/fcvm.2021.687585
Iqbal AM, Lopez RA, Hai O. Antiplatelet Medications. [Updated 2022 Nov 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537062/
Signs or circumstances that suggests a course of action should be taken. Term used in drug referencing to identify a particular use of a medication. For example, a beta blocker is indicated for the treatment of hypertension and angina. Or in stress testing perhaps chest pain is an indication for stopping the test.
A substance or drug chemical that binds to a receptor and blocks its activation, preventing a biological response.
A substance or drug chemical that binds to a receptor and results in a biological response. Agonists can cause a full response or a partial response (called sympathomimetic)
A symptom related to heart disease. Characterized by pain in the chest, jaw, shoulder or back. The pain is a result of a lack of oxygen delivered to the heart. It can be transient from a mismatch in oxygen demand and supply to the heart or occur during a myocardial infarction.
An abnormality of the heart in rhythm or rate. Synonymous with dysrhythmia
Inotrope is in reference to the strength of cardiac contraction. Negative inotrope = weaker, positive= stronger
Inotropy refers to the contractile strength or force of cardiac muscle cells, particularly in relation to the heart's function.
The stretch or filling of the heart chambers during the diastolic phase. This represents a load that must then be ejected during systole. Venous return influences preload, and in cases of heart failure, extra fluid retained can cause a heavy preload that overstretched the ventricle, causing added work for the heart, and reducing its ability to contract.
The resistance in the systemic circulation the ventricle must overcome to eject blood (systole). It is dependent on blood volume, blood viscosity and blood pressure. A stiff aortic valve can also be a source of resistance.
Metabolic Equivalent. A term used to describe metabolism and oxygen consumption by a huma. I MET equals 3.5 ml/kg/min of oxygen use. The cost of activities can be quantified by how many METs is required to perform the activity or exercise intensity.
A reduction in blood potassium. This can occur due to excessive potassium intake, diuretic use, vomiting and diarrhea, excessive seating or kidney disorders.
A condition of elevated levels of blood calcium. This may occur due to hyperparathyroidism, high calcium intakes, and diuretic use.
High levels of blood glucose. Hyperglycemia during a fasted measurement is seen in diabetic patients and represents either a failure to produce insulin (type I) or an impairment in the insulin- insulin receptor binding (type II). Some symptoms of hyperglycemia include increased thirst, frequent urinations, fatigue, dry mouth, and headaches.
A condition of low blood levels of sodium. This can occur due to dehydration, excessive water intake and medication use (thiazide diuretics)
The increased production of urine by the kidneys leading to increased urine output. Diuresis may be in response to increased blood pressure hormonal regulation to balance electrolytes or some medications such as diuretics.
The percentage of blood ejected from the left ventricle relative to the end diastolic volume. It is a key measure of heart contraction strength. EF= (stroke volume/ EDV) x 100
