2 Cardiac Related Conditions Commonly Seen in Cardiac Rehab
Before getting into the details about heart rhythms, medical interventions, and exercise prescription, it might be a good idea to do a quick overview of common cardiac conditions that the clinical exercise physiologist will be working with. This chapter is only meant to briefly introduce the conditions, and not to discuss pathophysiology. More will be discussed in later chapters.
Atherosclerosis: it’s everywhere!
Vascular disease begins the day we are born. Progressive damage, inflammation, and cholesterol plaque accumulation in blood vessels throughout the body are present in everyone. However, the rate of progression will vary, based on lifestyle and risk factors, such as:
- Sedentary lifestyle
- High Blood pressure
- Dyslipidemia (high LDL, low HDL cholesterol)
- Tobacco use
- Diabetes
- Obesity
Given the high proportion of individuals that are overweight, inactive, and metabolically unstable, it is no wonder that cardiac disease is the leading killer of men and women.
Vascular disease is not limited to the heart. It is within all blood vessels! Therefore, risk of stroke as well as peripheral artery disease often accompanies the cardiac patient, along with a multitude of ongoing risk factors. This makes treatment of the patient more difficult, as there are many different interacting problems.
Coronary arteries are quite small, so the accumulation of atherosclerotic plaque that occurs in blood vessels may make their presences known first in these blood vessels. As occlusions grow, opportunities arise to block flow in the blood vessels completely. This may occur because of a thrombus (blood clot) or atherosclerotic plaque that ruptures away from the vessel wall and lodges itself downstream. This complete occlusion results in an acute myocardial infarction. Since flow is blocked downstream from the occlusion, location matters!
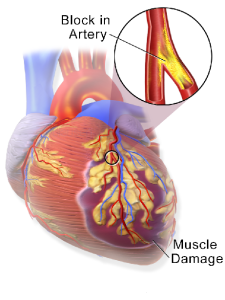
If the occlusion is towards the end of the coronary artery, the infarct may only affect a small portion of heart muscle. However, if the occlusion occurs near the origin of the artery, then a massive amount of heart muscle will die, and the person may not survive the infarction. Rapid response of emergency systems, and methods to reopen to blockage (i.e. thrombolytic medications, angioplasty) are essential. The myocardial infarction, or “MI” patient may have additional interventions performed prior to entering cardiac rehab, and conditioning the heart muscle to help it recover from the MI will be an essential component of rehab.
Peripheral Artery Disease
Another location for vascular disease to manifest is in the small blood vessels of the periphery, the limbs. Most often this occurs in the lower legs. Oxygen rich blood supply to the limbs is restricted, and as a result the muscles rely on anaerobic metabolism to produce the ATP for work. The result is a large accumulation of lactic acid in the lower limbs, accompanied by pain (known as Claudication). Movement is typically very restricted in these individuals, where they will feel pain within minutes of movement .
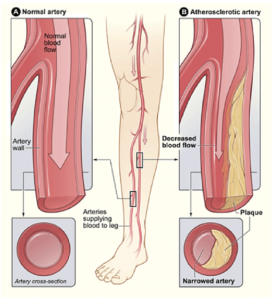
Recovery only comes by resting to allow clearance of blood from the affected area. Exercise physiologists can assess blood flow in the limbs using a pulse doppler along with a blood pressure cuff and measure the ankle brachial index. Individuals with peripheral artery disease are at risk of losing their limb, due to infection and lack of wound healing. So, exercise will be a very important part of their rehabilitation! Exercise for these individuals will be done in short intervals, with the goal of revascularizing the limbs to provide more blood flow to the tissue.

Heart Failure
Heart failure is the progressive failing of the heart as a pump to eject blood into systemic circulation. Ejection fraction drops over time, resulting in a reduced ability to do physical work, severe deconditioning, fluid retention and edema and ultimately death. There are a number of causes, but hypertension is a major factor in most cases.
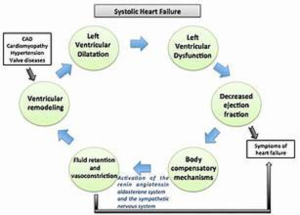
Patients will display symptoms of dyspnea, have elevated resting heart rates, and are probably taking diuretic medication, among other things. Exercise planning and symptom monitoring of these patients will be unique. Monitoring oxygen saturation will be an important factor with these patients due to the impaired diffusion of oxygen with pulmonary edema.
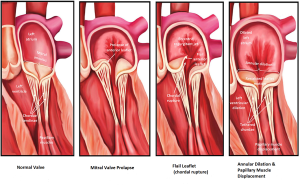
Valve Disorders
Since the heart is a series of 4 chambers, and blood flow needs to move in one direction, heart valves are essential to sealing the chambers at one end, while allowing blood to move out of the chamber in the desired direction. Valvular heart disease manifests in one of more of the heart valves. The mitral and aortic valves on the left side of the heart, and the pulmonic and tricuspid valve on the right side of the heart. Conditions typically relate to the valve not opening properly due to a valve stenosis (i.e. calcification) or perhaps regurgitation of blood backwards through a valve because it is not closing properly (i.e. mitral valve regurgitation or prolapse). The valve disorder can greatly affect heart function, such as ejection fraction and may also precipitate heart arrhythmias. The underlying causes can range from infection to heart disease. Fortunately, today’s medical technology has methods of replacing defective heart valves, so post-surgical patients can enter cardiac rehab to begin to train their heart to regain its conditioning .
Heart Dysrhythmias in the Ventricle and the Atria
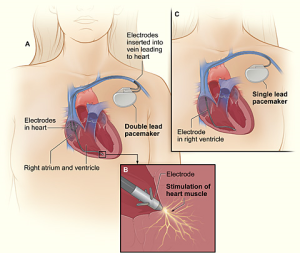
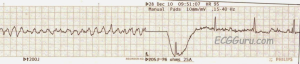
Heart arrhythmias can occur under a variety of circumstances, and may be congenital in nature, or related to heart disease. In some cases, arrhythmias can be fatal, such as ventricular tachycardia and ventricular fibrillation. To save the individual, shocking the heart using an AED (automated external defibrillator) may be the only solutions. There are some cardiac patients prone to fatal heart arrhythmias or simply need help pacing their heart due to conduction defects in the heart’s electrical system. For this reason, patients may have pacemaker installed in their chest and heart, often along with an internal defibrillator.
Atrial Fibrillation
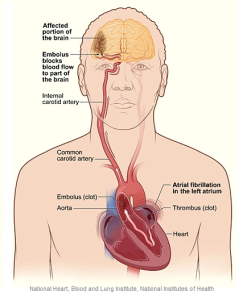
Fibrillation can also occur in the atria, often originating around the pulmonary veins in the left atria. Instead of a single sinus beat, where both atria contract to move blood to the ventricle, many cells in the atria are firing randomly, resulting in no atrial contraction.
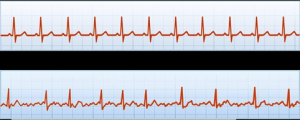
If the atria are not contracting, blood will pool in some pockets of the atrial (left atrial appendage). Pooling blood forms clots, which can be pushed into the aorta and to the brain causing a stroke. Treatments are to get the patient out of “afib” as soon as possible, try to isolate the initiating tissue and treat patients with medications designed to prevent blood clots.
Exercise physiologists may work with any or all the cardiac conditions identified in the overview. In-depth knowledge of the condition, related ECG information, medications and any symptomology are all important to effectively treat the patient.
Selected Sources
Clinical Exercise Physiology 5th ed. Ehrman, J et al. Human Kinetics ISBN -10 1718200447 2022.
Cardiac Rehabilitation (Contemporary cardiology) Krause and Keteyian Humana Pub. ISBN-10 1588297705 2007.
A chronic, inflammatory disease characterized by a buildup of cholesterol-laden plaque on the interior of the arteries, ultimately reducing blood flow to vital organs.
Often called a “heart attack” is when a coronary artery is blocked and blood flow to a portion of the heart is stopped, leading to cell death.
Refers to the complete blockage of a blood vessel or other tubular structure. Sometimes coronary artery degree of blockage is referred to as a percent occlusion. Sometimes used synonymously with the term “Stenosis.”
A blood clot that forms in a blood vessel or in the heart.
Refers to the complete blockage of a blood vessel or other tubular structure. Sometimes coronary artery degree of blockage is referred to as a percent occlusion. Sometimes used synonymously with the term “Stenosis.”
Pain or cramping in the legs during physical activity. The pain usually resolves with rest. Most often this pain is due to peripheral artery disease and is caused by local ischemia and the accumulation of lactic acid.
The percentage of blood ejected from the left ventricle relative to the end diastolic volume. It is a key measure of heart contraction strength. EF= (stroke volume/ EDV) x 100
Difficulty breathing characterized by breathlessness and a feeling of not being able to get enough air in the lungs to relieve the distress. Causes can include COPD, anxiety, deconditioning, and edema caused by heart failure.
The abnormal narrowing of a tubular structure, such as a coronary artery. Sometimes used synonymously with the term” Occlusion.”
An abnormality of the heart in rhythm or rate. Synonymous with dysrhythmia
